ACR CONVERGENCE 2020—Rheumatologists and patients have struggled with a lack of new therapies for systemic lupus erythematosus (SLE), but a better understanding of the underlying mechanisms behind the disease helps shed light on potential treatments.
ACR CONVERGENCE 2020—Rheumatologists and patients have struggled with a lack of new therapies for systemic lupus erythematosus (SLE), but a better understanding of the underlying mechanisms behind the disease helps shed light on potential treatments.
That was the theme of the ACR Convergence session State of the Art: Lupus—The Future Is Now, led by Peggy Crow, MD*, the Benjamin M. Cohen Chair in Immunology and Inflammation Research at the Hospital for Special Surgery and professor of medicine at Weill Cornell Medical College, both in New York City.
Genetic variations and ancestry frequently contribute to the development of lupus, Dr. Crow said. One area she addressed was gene expression differences in healthy African Americans vs. European Americans. Two recent studies found African Americans were more predisposed to produce anti-ribonucleoprotein (anti-RNP) and anti-double-stranded DNA (anti-dsDNA) autoantibodies. In contrast, European Americans were predisposed to make only anti-dsDNA autoantibodies. These transancestral pathways reflect the role of interferons and pathways that are connected to tissue repair and remodeling, Dr. Crow explained.1,2
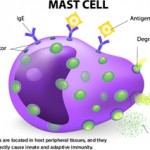
The pathogenesis of lupus often involves pathways from the innate immune system, as well as autoantibodies, Dr. Crow stated. “I think you need both to lead to clinical disease,” she said.
Environmental factors also play a role in the development of SLE, and Dr. Crow presented research on the influence of such factors as smoking. In a study with 673 SLE patients and 3,272 controls, a high genetic risk score and current or recent smoking status were strongly associated with a risk for developing lupus.3
Dr. Crow also addressed the role of type 1 interferon and its role in SLE. She described type 1 interferon as “a smoldering fire for immune system activation.” One finding from Dr. Crow et al. is that the transcription factor IRF5 is a key mediator of endosomal toll-like receptor induction of type 1 interfeon.4 Type 1 interferon appears to contribute to the clinical signs of SLE, including autoimmunity, inflammation and skin rashes, she said.
With COVID-19 under investigation by many scientists right now, Dr. Crow drew parallels between some of the findings on COVID-19 and the innate immune response and lupus. These occur even though a virus is not the driver behind SLE. “Maybe we can learn a lot from both diseases,” she stated.
Potential Targets for Lupus Therapy
Hydroxychloroquine remains the foundational treatment for SLE, but other treatments are under investigation, Dr. Crow reported. Toll-like receptor 7 as a therapeutic target has been previously reported (“PAD2 & PAD4 Modulate Immune Response in TLR-7-Dependent Lupus”). Other therapies with recent results include anifrolumab and Janus kinase inhibitors that target kinases downstream from the type 1 interferon inhibitor receptor. Both of these therapies inhibit downstream effects and not interferon itself, Dr. Crow said.