SEBASTIAN KAULITZKI/Science Source
When rheumatologists think about rheumatoid arthritis (RA), they are apt to picture the synovium, contemplate such antibodies as rheumatoid factor and those to citrullinated proteins, and consider how this interplay of factors manifests in disease. What is not as commonly discussed is the role the autonomic nervous system plays in the pathogenesis and symptomatology of RA.
Evaluating Autonomic Function
In 2014, a group of researchers sought to evaluate autonomic function in RA as a potential mechanism by which the disease can increase cardiovascular mortality. The authors ultimately demonstrated that autonomic nervous system (ANS) dysfunction was present in about 60% of patients with RA across the 40 studies included in the review.1 Such a finding is important because, beyond its effects on the cardiovascular system, the ANS also appears to play a significant role in regulating inflammation in animal models and humans.2,3
The association between ANS dysfunction and RA raises an important question: Is the ANS imbalance a result of chronic inflammation, or do changes in the ANS affect inflammation, disease development and severity of RA?
The answer to that question is not clear, according to Matthew Baker, MD, MS, clinical assistant professor and clinical chief, Division of Immunology and Rheumatology, Stanford University, Palo Alto, Calif., and Mark Genovese, MD, senior vice president, inflammation, at Gilead Sciences Inc., Foster City, Calif. However, Dr. Baker notes the research cited above and anecdotal observations of improved RA symptoms on the side of hemiparesis in patients who have had stroke have inspired further evaluation of the neurologic/immunologic connection in RA.
The Science
Two studies have been conducted in recent years with implantable vagus nerve stimulation devices as a possible treatment for RA. These studies demonstrate improvements in systemic inflammation and disease activity and show good safety profiles for these devices.4,5
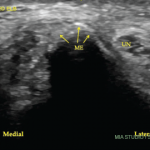
To build on this work, a proof-of-concept study was conducted of a noninvasive vagus nerve stimulation device for the treatment of patients with RA. Thirty patients with active RA and an inadequate response to treatment with disease-modifying anti-rheumatic drugs (DMARDs) were enrolled in the study. Active disease was defined as a Disease Activity Score of 28 joints with C-reactive protein (DAS28-CRP) of >3.8, with four or more tender joints and four or more swollen joints on 28 joint count and any active osteitis or articular synovitis in the wrist or hand as confirmed by ultrasound or magnetic resonance imaging (MRI). An inadequate response was defined as patients who had tried one or more conventional synthetic DMARDs for at least 12 weeks, including with a stable dose for four weeks or longer before enrollment, or had failed to respond to or did not tolerate one biologic DMARD. Biologic DMARDs were discontinued at least four weeks prior to the start of the trial, and use during the trial was not permitted.
Eligible participants were assigned to use a noninvasive, wearable vagus nerve stimulation device that generated electrical pulses that were then delivered transcutaneously to the external ear. Patients were asked to use the device for up to 30 minutes each day and were restricted from making adjustments to stimulation parameters. The earpieces for the devices were personalized to fit each patient comfortably and the device logged patient usage to track compliance.
Baseline measures of RA activity included DAS28-CRP, the Health Assessment Questionnaire-Disability Index (HAQ-DI), MRI, ultrasound, blood analyses and a sleep quality assessment. Follow-up visits took place at weeks 1, 2, 4, 8 and 12. The primary endpoint in the study was mean change in DAS28-CRP at week 12 compared with baseline, and secondary endpoints included safety analysis; the proportion of patients achieving ACR20, ACR50 and ACR70 responses; the proportion of patients achieving a difference of 0.22 on HAQ-DI at week 12; and mean change in HAQ-DI at week 12.
Two studies have been conducted in recent years with implantable vagus nerve stimulation devices as a possible treatment for RA. These studies demonstrate improvements in systemic inflammation & disease activity.
Of 30 patients enrolled in the study, 27 completed the week 12 visit. Patients used the device on 94% of the study days, and this measurement of compliance has high validity given that compliance was automatically tracked by the devices. A significant reduction was seen in DAS28-CRP after week 1 and this score remained significantly reduced at week 12. Some 37% of patients reached DAS28-CRP of 3.2 or less, which indicates low disease activity, and 23% of patients reached DAS28-CRP of less than 2.6, which indicates remission, at week 12. In addition, 53% of patients reached ACR20, 33% reached ACR50 and 17% reached ACR70. With respect to imaging, the mean change in ultrasound synovitis and tenosynovitis scores were statistically significant and, for MRI, reductions in synovitis, osteitis, bone erosion and cartilage loss scores at week 12 compared to baseline were seen, although these were not statistically significant.6
Lead author Sara Marsal, MD, associate professor of rheumatology and head of rheumatology, Vall d’Hebron University Hospital, Autonomous University of Barcelona, Spain, summarizes the key clinical takeaways from this study. “The proof-of-concept clinical data show meaningful clinical benefit for the majority of participants, as assessed by the usual clinical endpoints (ACR20/50/70 and DAS28-CRP) and a very favorable risk/benefit profile,” Dr. Marsal explains. “Seeing low disease activity and remission for some patients was encouraging. Imaging of the joints with ultrasound, which is common practice in Europe, reinforced the benefit.”
In discussing the study results, Dr. Baker notes that patient compliance with the device was high, as were patient satisfaction scores. He explains that because the earpieces were custom-molded for each patient and the treatment is designed to be imperceptible, it is a comfortable experience for the patient. In addition, very few adverse events occurred; in fact, the only device-related event was a superficial skin abrasion in one patient. Given that customization of devices is quick and inexpensive, it would be expected that this would be possible even if and when the devices are available for widespread use. Such customization improves comfort for patients and helps ensure proper functioning.
It is important to understand potential limitations of this study, including some of the trial’s exclusion criteria. Patients with a history of previously implanted electrically active medical devices, such as cardiac pacemakers or automatic implantable cardioverter defibrillators, were excluded from participation. Because this was the first open-label pilot study of this noninvasive vagus nerve stimulation device, Dr. Genovese explains, it made sense to exclude these patients out of an abundance of caution. However, it would be reasonable to think the stimulation device could be safely used in these patients in the future and that such patients may not necessarily be excluded from larger future trials but preliminary studies in this population would need to demonstrate no cross interference.
In addition, the patient population in this study was predominantly naive to biologic DMARDs, thus it is not known if the benefits of treatment with the device would be seen in patients who are refractory to biologic DMARD or targeted synthetic DMARD treatment. Finally, vagus nerve stimulation was not combined with treatment with biologic or targeted synthetic DMARDs; thus, it is unknown if a potential additive effect of these treatments could occur when used together.
Dr. Genovese provides helpful insight, stating, “Although limited conclusions can be reached from open label studies and those with relatively small numbers of patients, one can’t help but be enthusiastic about the possibility of noninvasive vagus nerve stimulation as an adjunctive treatment in helping reduce some of the symptoms associated with RA.”
John Miller, MD, an instructor of medicine in the Johns Hopkins Arthritis Center, notes, “While there are inherent limitations in a pilot study like this, the results are compelling and warrant further examination in a randomized process, particularly with an adequate placebo group.
“If these data are replicated in larger studies,” he adds, “it will also be important to determine which subsets of patients respond best to therapy. Other teams have shown similar results with vagal nerve stimulation, though there was suggestion that response may be related to underlying disease activity.”7
Noninvasive vagus nerve stimulation is worthy of further exploration as a potential treatment in RA.
Next Steps
Dr. Marsal notes that the next step in research on this subject would be to further validate the results from this study by conducting properly controlled, randomized clinical trials. Dr. Baker and Dr. Genovese indicate the company that produces the device will be directing a sham-controlled study in the U.S.
Much remains to be learned about the neurologic/immunologic connection in RA, and this study helped shed some light on the subject and provide evidence that noninvasive vagus nerve stimulation is worthy of further exploration as a potential treatment in RA.
Researchers will be able to help advance the field of rheumatology by rigorously evaluating novel treatments like vagus nerve stimulation and—as long as they have the nerve to do so—can help many patients in the process.
Jason Liebowitz, MD, completed his fellowship in rheumatology at Johns Hopkins University, Baltimore, where he also earned his medical degree. He is currently in practice with Skylands Medical Group, N.J.
References
- Adlan AM, Lip GYH, Paton JFR, et al. Autonomic function and rheumatoid arthritis: A systematic review. Semin Arthritis Rheum. 2014 Dec;44(3):283–304.
- Pavlov VA, Tracey KJ. Neural regulation of immunity: Molecular mechanisms and clinical translation. Nat Neurosci. 2017 Feb;20(2):156–166.
- Evrengül H, Dursunoglu D, Cobankara V, et al. Heart rate variability in patients with rheumatoid arthritis. Rheumatol Int. 2004 Jul;24(4):198–202.
- Koopman FA, Chavan SS, Miljko S, et al. Vagus nerve stimulation inhibits cytokine production and attenuates disease severity in rheumatoid arthritis. Proc Natl Acad Sci U S A. 2016 Jul 19;113(29):8284–8289.
- Genovese MC, Gaylis N, Sikes D, et al. Safety and efficacy of neurostimulation with a miniaturised vagus nerve stimulation device in patients with multidrug-refractory rheumatoid arthritis: A two-stage multicentre, randomised pilot study. Lancet Rheumatol. 2020 Sept 1;2(9):E527–538.
- Marsal S, Corominas H, de Agustín JJ, et al. Non-invasive vagus nerve stimulation for rheumatoid arthritis: A proof-of-concept study. Lancet Rheumatol. 2021 Apr 1;3(4):e262–269.
- Drewes AM, Brock C, Rasmussen SE, et al. Short-term transcutaneous non-invasive vagus nerve stimulation may reduce disease activity and pro-inflammatory cytokines in rheumatoid arthritis: Results of a pilot study. Scand J Rheumatol. 2021 Jan;50(1):20–27.