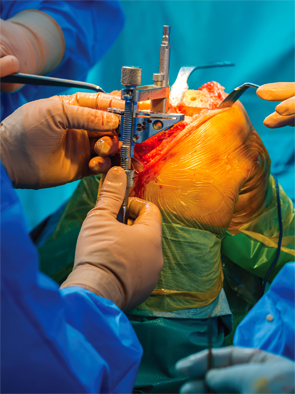
egyjanek/shutterstock.com
A study that looked at the impact of hepatitis C on short-term outcomes of total joint arthroplasty found an increase in co-morbidity compared with patients without the liver disease.
The number of people in need of total joint arthroplasty is expected to rise in conjunction with an aging population and advances in hepatitis C treatments. With this in mind, the study aimed to assess the association between hepatitis and perioperative outcomes of lower-extremity total joint arthroplasty, the authors note in a study published in The Journal of Bone & Joint Surgery.1
“Awareness is growing among arthroplasty surgeons that hepatitis is becoming increasingly common among patients getting surgery to replace hip or knee joints,” says co-author Michael Mont, MD, director of joint preservation and reconstruction for LifeBridge Health, Baltimore.
Rising Problem
“For example, from 1998 to 2010, the number of patients who were getting total joint arthroplasties who have hepatitis C infection tripled,” Dr. Mont says. Results also showed that these patients had an increased risk of medical and surgical complications and stayed longer in the hospital after the operation compared with patients in the study from the matched control group.
Chronic infection of hepatitis C can severely damage the liver, and it may also contribute to the development of rheumatoid arthritis. Baby boomers born between 1945 and 1965 are at higher risk for hepatitis C, according to the Centers for Disease Control and Prevention. Because they are an aging population, they are also more likely to undergo hip arthroplasty.
The Study

Dr. Mont
Researchers involved in the study identified patients who underwent either a total hip or knee arthroplasty in the U.S. from 1998 to 2010, using the Nationwide Inpatient Sample database. They matched controls in a three-to-one ratio to patients with hepatitis C infection according to surgical procedure, age, race, sex, Deyo comorbidity score and year of surgical procedure. Outcomes included perioperative complications (any, medical, surgical) and mean length of stay.
Out of a database of some 1.7 million arthroplasty patients, researchers identified and reviewed the outcomes of about 8,000 patients who had hepatitis C and had joint arthroplasties.
“What we found was not incredibly surprising, that patients who have hepatitis C have more complications after getting a hip or knee arthroplasty,” Dr. Mont says.
Overall, patients with hepatitis C were 30% more likely to have any type of complication and were 15% more likely to have a medical complication. Most notably, risks for surgical complications were 78% higher among patients with hepatitis C than matched controls. The surgical risks, which include complications such as infections, may be associated with multi-organ complications common in patients with the virus, according to the article.
The 30% rise in the number of joint replacements among patients with hepatitis C was not merely a reflection of a general upswing over the years in these types of operations, says Dr. Mont. Taking into account the number of operations among the general population, the frequency of hepatitis C infection rose from 1.9 per 1,000 total joint arthroplasties in 1998 to 5.9 per 1,000 total joint arthroplasties in 2010.
Previous Studies
Earlier studies that were smaller and conducted at single centers have shown similar findings, Dr. Mont explains. So even though results of the most recent study were somewhat expected, they do help further clarify some concerns facing patients with hepatitis C who have compromised immune systems and may be more susceptible to infection if they undergo surgery, he says.
Orthopedic surgeons should be aware of the increased risks of total joint arthroplasty in patients with hepatitis C & should discuss these risks with potential surgical candidates during a shared decision-making process.
“It’s just defining it a little bit better,” Dr. Mont explains. “We would expect that people who have had hepatitis are going to be more immunocompromised, more subject to vasculitis” and more subject to adverse effects on all of their organ systems, he says.
Future studies are needed to determine whether adopting strict measures to optimize the medical health of a patient infected with hepatitis C could lead to reduced complications from hip or knee arthroplasty, Dr. Mont says.
Conclusions
The authors concluded that hepatitis C infection is an infrequent but increasingly common co-morbidity among patients who undergo total joint arthroplasty.
“Given these findings, orthopaedic surgeons should be aware of the increased risks of total joint arthroplasty in patients with hepatitis C and should discuss these risks with potential surgical candidates during a shared decision-making process,” the authors write in the study.
Insight gained from the study is useful in the counseling of patients with hepatitis C about their increased risks when considering a total joint arthroplasty procedure, according to the authors of a separate commentary that appears in the same journal issue as the study article.2
“An awareness of the need for and benefit of patient education, medical optimization and utilization of a medical or surgical care team approach could help to decrease the complication rate associated with total joint arthroplasty in this population,” write Pooya Javidan, MD, and Richard H. Walker, MD, of the Scripps Clinic in La Jolla, Calif.
Catherine Kolonko is a medical writer based in Oregon.
References
- Issa K, Boylan MR, Naziri Q, et al. The impact of hepatitis C on short-term outcomes of total joint arthroplasty. J Bone Joint Surg Am. 2015 Dec 2;97(23):1952–1957.
- Javidan P, Walker RH. Take care with type C: Serious considerations in the selection of patients with hepatitis C for total joint arthroplasty: Commentary on an article by Kimona Issa, MD, et al.: ‘The Impact of Hepatitis C on Short-Term Outcomes of Total Joint Arthroplasty.’ J Bone Joint Surg Am. 2015 Dec 2;97(23):e77.

