
shepele4ek2304 / shutterstock.com
For people with rheumatoid arthritis (RA), fatigue can be a debilitating symptom that interferes with daily life and significantly reduces quality of life. Managing fatigue can be difficult; it is linked to disease activity and a host of other conditions that commonly accompany RA, such as depression, sleep problems and obesity.
A new study, however, suggests that use of a simple intervention can have a significant impact on reducing fatigue by targeting a common source of fatigue in people with RA—that is, physical inactivity.
A recent study by Katz and colleagues found that patients with RA who used a pedometer to monitor their physical activity had a significant reduction in fatigue.1 In addition, increasing physical activity also improved self-reported disease activity, functioning, depression and pain interference.
“Pedometers have been used in a lot of studies to improve activity, and they generally are effective, because when you are monitoring your behavior, it is a lot easier to change it,” says lead author of the study, Patricia Katz, PhD, professor, Department of Medicine University of California, San Francisco, Arthritis Research Group, San Francisco.
A key take-home message for patients with RA is that moving more is good for you. “The study shows that moving more doesn’t make RA worse, but does improve fatigue and other aspects of the disease,” says Dr. Katz.
A Closer Look

Dr. Katz.
The study was undertaken by Katz and colleagues based on data gleaned from a previous study that showed inactivity as a key source of fatigue for people with RA.2 To test whether increasing physical activity could improve fatigue, 96 patients with RA were randomized to one of three treatment groups and followed for 21 weeks. Table 1 describes the intervention used in each treatment group.
All patients had well-established disease with comparable self-reported disease activity and levels of functional impairment at baseline. Most were female (88%), white (64%) and had a mean age of 54 years. Of the total group, 22% were Spanish speaking. The only significant baseline differences among the three groups was that patients in the placebo group were older and had a longer duration of RA.
Based on the changes in weekly average number of daily steps (primary outcome), the study found that patients in both intervention groups significantly increased their physical activity, as demonstrated by an increase in average daily steps (+1,441 for PED and +1656 for PED+; P=0.004 and P=0.001, respectively).
Using the Patient-Reported Outcomes Measurement Information System (PROMIS) to measure fatigue, patients in both intervention groups also had a significant reduction in fatigue after 21 weeks compared with baseline scores (-3.2 for PED and -4.8 for PED+; P=0.02 and P=0.0002, respectively). No statistically significant differences were seen between the two intervention groups.
Patients in the placebo group, however, had no change in their physical activity and actually demonstrated decreased activity (-747 steps; P=0.14) and no improvements in fatigue (-1.6; P=0.26). (All patients in the study had a week of activity monitoring prior to randomization and another week of monitoring at the end of the study. The decreased activity noted in the placebo group is based on a comparison of the measurements of these two weeks of activity monitoring in this group.)
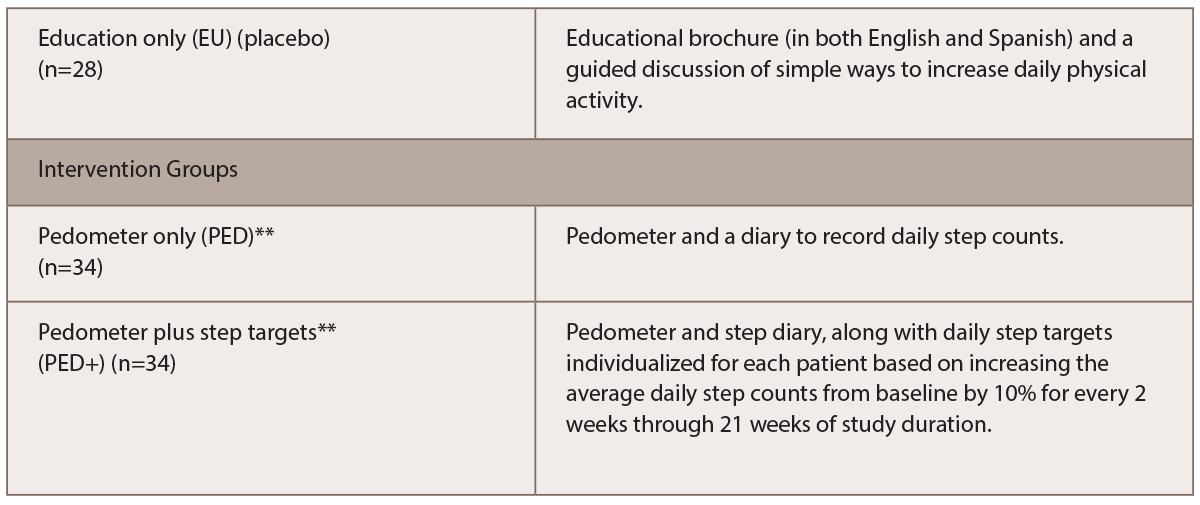
(click for larger image) Table 1: Treatment Groups*
* Patients in all three groups received an educational booklet and discussion about ways to increase daily physical activity.
** Patients were contacted every two weeks to collect recorded steps.
Along with showing significant improvements in physical activity and decreases in fatigue in the patients who wore pedometers, the study also found that patients who wore pedometers had significant improvements in self-reported disease activity, pain interference and depressive symptoms.
Dr. Katz emphasized that all of these improvements, along with the significant decrease in fatigue, were achieved simply by having patients wear pedometers to monitor their activity and instructing them to walk more. “We didn’t give an instruction on intensity or anything else,” she said. “The directive was just to walk more.”

Dr. Iversen.
Commenting on the study, Maura Daly Iversen, PT, professor and director of Rehabilitation and Epidemiology Trainee Program, Department of Physical Therapy, Movement & Rehabilitation Sciences, Northeastern University, Boston, suggests the simplicity of using pedometers may offer a needed approach to improving fatigue in RA patients.
“Fatigue is a well-known symptom in RA, but is often under-appreciated clinically,” says Dr. Iversen, who is also associate dean of new initiatives, Bouve College of Health Sciences. “A number of self-management programs provide strategies to help patients manage their fatigue via [such methods as] cognitive behavioral therapy (CBT), counseling, sleep hygiene, exercise and recommendations for physical activity (PA), but these can be time intensive for patients and resource intensive for clinics.”
This well-designed randomized controlled trial, she says, shows that pedometers “used with phone contacts to gather data increases physical activity among adults with established RA and that this increase in physical activity has positive effects on fatigue, as well as other RA-related symptoms.”
Get Patients to Move More
For clinicians who counsel patients with RA on how to manage fatigue and other RA-related symptoms, the study highlights the importance of getting patients to move more. To do this, Dr. Katz emphasizes the need for clinicians to offer a bit more guidance on how to increase physical activity beyond simply telling them to exercise more. Only offering educational information and discussion on the need to exercise is ineffective, as highlighted by the patients in the placebo group who actually decreased their level of physical activity.
Instead, Dr. Katz underscores the need to provide patients with some direction about making incremental changes to their physical activity levels. “Basically, when people hear they need to exercise, they think they need to go to the gym and need to work out hard,” she says. “But I think that giving people something that is approachable and with an attainable goal is good.”
Given that most people have smartphones with activity trackers, she says an easy way to get patients moving more is to counsel them to use such trackers or pedometers to increase their daily steps by minor increments. “Anything helps,” she says.
Mary Beth Nierengarten is a freelance medical journalist based in Minneapolis.
References
- Katz P, Margaretten M, Greogorich S, Trupin L. Physical activity to reduce fatigue in rheumatoid arthritis: A randomized controlled trial. Arthritis Care Res (Hoboken). 2018 Jan;70(1):1–10.
- Katz P, Margaretten M, Trupin L, et al. Role of sleep disturbance, depression, obesity, and physical inactivity in fatigue in rheumatoid arthritis. Arthritis Care Res (Hoboken). 2016 Jan;68(1):81–90.

