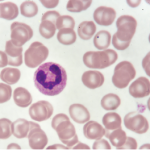
ALIOUI MA / shutterstock.com
Neutrophils, often hailed as guardians against infections, are maligned when it comes to rheumatoid arthritis (RA) due to their role in both the initial stage and disease progression. A new multicenter work, “A Neutrophil Activation Biomarker Panel in Prognosis and Monitoring of Patients with Rheumatoid Arthritis,” seeks to expand the literature on this topic.1 The study, published in Arthritis & Rheumatology, examines whether neutrophil activation markers might be helpful in the diagnosis, prognosis and monitoring of RA patients.
Co-author Christian Lood, PhD, assistant professor in the Division of Rheumatology, Department of Medicine, University of Washington, Seattle, notes, “Under normal conditions, neutrophils are terrific immune cells that will defend against any type of microbe. One of the many ways a neutrophil can combat intruders is through the formation of neutrophil extracellular traps (NETs), also called NETosis. NET formation is a process by which DNA and other antimicrobial agents are ejected from the neutrophil in a sticky net that traps and kills pathogens. The problem for those with RA is that if all of the NET fragments are not removed, then autoantibodies directed against NET-related proteins and DNA can form, resulting in the development of RA (or lupus).
“My co-authors and I wanted to explore whether NETs are present in the circulation of RA patients and the extent to which they contribute to inflammation and disease progression,” he says.
A Close Look at Cellular Death
“During NETosis, the amino acid arginine is converted into citrulline, an event that makes the immune system of RA patients run amok, identifying the citrullinated self-molecules as foreign. The formation of these antibodies toward citrullinated peptides, ACPA, is used clinically for RA diagnosis,” Dr. Lood explains.
“In healthy individuals, NETs are promptly removed from the circulation. However, RA patients have a lower capacity to degrade the NETs, which is why they are essentially left hanging around; this induces inflammation and organ damage,” he notes.
“Prior studies have indicated that RA patients may have elevated levels of NETs in serum samples,” says Dr. Lood. However, he notes that because the neutrophils are fragile and undergo NET formation upon serum processing, assessing serum levels alone may not reflect the true physiological levels of neutrophil extracellular traps in RA patients.
Dr. Lood
‘By combining existing panels with this neutrophil marker, we will have a much better ability to identify patients at high risk of the most devastating forms of RA.’ —Christian Lood, PhD
To address this gap in the literature, Dr. Lood and his colleagues studied 101 patients with RA who were age- and gender-matched with 20 healthy participants. Disease activity was recorded using the CDAI (Clinical Disease Activity Index) for RA, taking into account tender and swollen joints, patient global assessment and provider global assessment.
“When we looked at plasma samples to determine the true levels of NETs in patient circulation, we found that RA patients had profoundly elevated levels of NETs as compared to healthy individuals,” Dr. Lood says. “Similarly, another marker of neutrophil activation, calprotectin, was useful in monitoring patients [because] it tracks very well with disease activity. In our study, both calprotectin and NETs were better than C-reactive protein in identifying patients with active RA.”
Commenting on the finding that NET levels are high even among RA patients in remission, Dr. Lood notes, “It was quite surprising to see patients with no signs of the disease have such a high degree of neutrophil activity. In fact, we found that levels of NETs, as well as calprotectin, predicted development of a common extra-articular disease modification—RA nodules—as well as erosive disease. Also concerning is that this low-grade inflammation may play a role in the development of cardiovascular disease.”
“The most exciting aspect of this work is that we can predict what will happen to patients,” Dr. Lood says. “If, at an RA patient’s initial visit, we find that he or she has this marker for NETosis, then we can predict long term if they will develop severe extra-
articular manifestations. If we can identify these patients early on, then we can be aggressive in trying to prevent joint disability.”
Personalized RA Treatment?
“Going forward,” says Dr. Lood, “we hope to recruit a large cohort of roughly 1,000 patients to validate these results. Ideally, this would be an international collaboration of patients from diverse backgrounds. We are also working with pharmaceutical companies to determine the utility of the neutrophil biomarkers in prediction of treatment responses, helping ensure that patients get adequate treatment without unnecessary side effects. This is getting us closer to personalized medicine.”
Dr. Lood stresses that “more national attention is needed to determine how we can use this information to help patients. Even in established patients we see that this marker tracks well with disease activity, so it definitely has value for many patients.”
In addition, Dr. Lood says, “We are working with a diagnostic company, Exagen, to further our understanding of the clinical utility of neutrophil biomarkers in rheumatic diseases, as well as develop assays for clinical use.
“By combining existing panels with this neutrophil marker, we will have a much better ability to identify patients at high risk of the most devastating forms of RA. In addition, such an approach provides us with an opportunity to stratify patients for clinical trials, treatment and disease monitoring,” Dr. Lood concludes.
Elizabeth Hofheinz, MPH, MEd, is a freelance medical editor and writer based in the greater New Orleans area.
Reference
- Bach M, Moon J, Moore R, et al. A neutrophil activation biomarker panel in prognosis and monitoring of patients with rheumatoid arthritis. Arthritis Rheumatol. 2020 Jan:72(1):47–56.