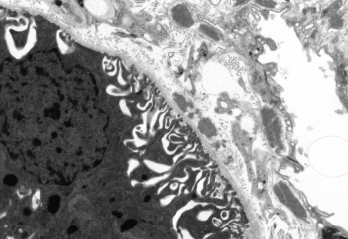
Patricia Navarro, Roger J. Bick, Brian J. Poindexter / UT-Houston Medical School/Science Source
Over time, systemic lupus erythematosus (SLE) can lead to considerable organ damage. Preventing this outcome is complicated by a scarcity of treatment options that can drive the disease into remission and by the side effects of existing therapies, such as prednisone and other corticosteroids, which may themselves contribute to the long-term damage.
The largest study to date comparing remission with lupus low disease activity state (LLDAS) as a predictor of organ damage has found that even a small percentage of time spent in clinical remission can give patients significant protection against organ damage.1 For patients who achieve the easier target of LLDAS for at least half the time on clinical follow-up, the risk of organ damage can still be cut in half.
An Achievable Goal
Lead author Michelle Petri, MD, MPH, director of the Hopkins Lupus Center and a professor of medicine at Johns Hopkins University School of Medicine, Baltimore, says her study reaffirms the clear benefits of remission while backing a more realistic treat-to-target strategy for rheumatologists. “Our current therapies just are not good enough to achieve remission. LLDAS offers an achievable outcome that will push us to treat to target,” Dr. Petri says. “LLDAS is easy to complete: It should be doable in the routine clinic setting and not overly burdensome to the rheumatologist in practice.”
Two independent rheumatologists say they agree with the study’s main conclusions. Ronald van Vollenhoven, MD, PhD, director of the Amsterdam Rheumatology and Immunology Center in the Netherlands, says he “really liked the study” and agrees that because LLDAS is more easily achievable and confers significant health benefits, it offers a reasonable outcome target.
“Having said that, both patients and expert physicians agree that, in the end, remission is desirable,” says Dr. van Vollenhoven, who is also chief of the Department of Rheumatology and Clinical Immunology at the Academic Medical Center and of the Department of Rheumatology at Vrije Universiteit Medical Center, Amsterdam. “Perhaps the two goals or targets could be combined in a long-term treatment strategy [in which] the patient is hopefully able to achieve LLDAS as a first step—and then move on to remission.”
Eric Morand, PhD, FRACP, head of the School of Clinical Sciences and a rheumatologist at Monash University’s Monash Health in Melbourne, Australia, likewise agrees with the study’s conclusions and notes that several other published clinical trials and abstracts have supported the attainability of treating to target for LLDAS. “Remission of course remains the goal, but just as in rheumatoid arthritis, it took both good measures and breakthrough medicines to establish remission as a feasible goal for usual care,” Dr. Morand says. “For now, LLDAS has the data behind it.”
Study Details
The study, published recently in Arthritis & Rheumatology, assessed data from 1,356 patients who had been followed quarterly within the Hopkins Lupus Cohort and who accounted for 77,105 person-months of observation from 1987 to 2016. In 13% of those person-months, the patient achieved clinical remission with no treatment, while 27% achieved clinical remission on treatment. By far the largest category, though, was LLDAS, which was reached in 50% of all person-months.



