Nationally, the U.S. is facing a physician shortage across all medical specialties. With an aging U.S. population increasing the need for care, rheumatology is no exception to this national trend. In 2005, the ACR conducted a formal workforce study, projecting the demand for rheumatology services would increase by approximately 46% but the supply of rheumatologists would increase by only about 1.2%.
New research into rheumatology’s supply and demand projections has integrated data from primary and secondary sources, estimating the baseline adult rheumatology workforce and determining demographic and geographic factors relevant to the rheumatology workforce. The study used a patient-centered approach that considered regional access to care. The study also estimated the clinical full time equivalents (FTEs) to better understand the clinical productivity of the workforce, which includes physicians, nurse practitioners and physician assistants. The findings of “2015 American College of Rheumatology Workforce Study: Supply and Demand Projections of Adult Rheumatology Workforce, 2015–2030,” published in the April 2018 issue of Arthritis Care & Research, mirror national projections and may aid in strategic planning and/or identifying potential strategies to mitigate workforce challenges.
The Projections
“The adult rheumatology workforce projections reflect a major demographic and geographic shift that will significantly impact the supply of the future workforce by 2030,” write the authors.
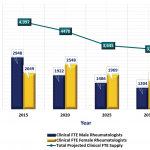
At baseline in 2015, the total number of adult rheumatology patient care providers was 6,013, with corresponding clinical FTEs of 5,415. Overall in 2015, the demand for rheumatologic care exceeded the supply of providers by 700 clinical FTEs (12.9%). Using data from the U.S. Census Bureau, researchers estimated that compound growth for demand from 2015–2030 to be approximately 2.5%, up 1.5% from the 2005 study. By 2030, the demand for rheumatologic care is projected to exceed supply by 4,133 clinical FTEs (102%).
Supply factors: Rheumatology has a growing number of providers moving toward retirement. Researchers note that changes in workload and an increase in the number of providers work fewer hours, the number of patients seen each week by physicians has decreased 14–19% (for male and female physicians, respectively) since 2005.
The number of future adult rheumatology providers depends on available fellowship positions, the fill-rate of those positions, graduation rates and the number of international medical graduates who plan to (or are allowed to) remain in the U.S. By 2030, projections indicate 4,346 (2,477 female/1,869 male) rheumatologists will be working in the U.S. The authors write, “Based on the workforce study model, the projected loss of clinical FTE due to retirees over the next 10 years greatly exceeds the capacity of rheumatology training programs to replace them with new graduates.”