Nationally, the U.S. is facing a physician shortage across all medical specialties. With an aging U.S. population increasing the need for care, rheumatology is no exception to this national trend. In 2005, the ACR conducted a formal workforce study, projecting the demand for rheumatology services would increase by approximately 46% but the supply of rheumatologists would increase by only about 1.2%.
New research into rheumatology’s supply and demand projections has integrated data from primary and secondary sources, estimating the baseline adult rheumatology workforce and determining demographic and geographic factors relevant to the rheumatology workforce. The study used a patient-centered approach that considered regional access to care. The study also estimated the clinical full time equivalents (FTEs) to better understand the clinical productivity of the workforce, which includes physicians, nurse practitioners and physician assistants. The findings of “2015 American College of Rheumatology Workforce Study: Supply and Demand Projections of Adult Rheumatology Workforce, 2015–2030,” published in the April 2018 issue of Arthritis Care & Research, mirror national projections and may aid in strategic planning and/or identifying potential strategies to mitigate workforce challenges.
The Projections
“The adult rheumatology workforce projections reflect a major demographic and geographic shift that will significantly impact the supply of the future workforce by 2030,” write the authors.
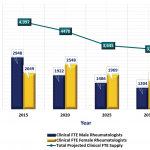
At baseline in 2015, the total number of adult rheumatology patient care providers was 6,013, with corresponding clinical FTEs of 5,415. Overall in 2015, the demand for rheumatologic care exceeded the supply of providers by 700 clinical FTEs (12.9%). Using data from the U.S. Census Bureau, researchers estimated that compound growth for demand from 2015–2030 to be approximately 2.5%, up 1.5% from the 2005 study. By 2030, the demand for rheumatologic care is projected to exceed supply by 4,133 clinical FTEs (102%).
Supply factors: Rheumatology has a growing number of providers moving toward retirement. Researchers note that changes in workload and an increase in the number of providers work fewer hours, the number of patients seen each week by physicians has decreased 14–19% (for male and female physicians, respectively) since 2005.
The number of future adult rheumatology providers depends on available fellowship positions, the fill-rate of those positions, graduation rates and the number of international medical graduates who plan to (or are allowed to) remain in the U.S. By 2030, projections indicate 4,346 (2,477 female/1,869 male) rheumatologists will be working in the U.S. The authors write, “Based on the workforce study model, the projected loss of clinical FTE due to retirees over the next 10 years greatly exceeds the capacity of rheumatology training programs to replace them with new graduates.”
The study also highlights the current and future maldistribution of adult rheumatologists practicing in the U.S., with 21% of rheumatologists in the Northeast compared with only 3.9% in the Southwest. “In 2015, the ratio of provider per 100,000 patients by region ranged from 3.07 in the Northeast to 1.28 in the Southwest,” note the authors. “By 2025, there is an anticipated decrease in all regions, ranging from 1.61 in the Northeast to 0.50 in the Northwest.”
In their discussion, the authors note the need for creative solutions. “These results represent a dramatic decline in the rheumatology workforce from 2015 to 2030,” they write. The authors also suggest potential strategies to address some of these workforce challenges, including recruiting nonphysician providers, encouraging changes in the regional distribution of the workforce, expanding telemedicine programs, retaining international medical graduates who train in rheumatology and improving practice efficiencies.
In response to the 2005 workforce study, the number of first-year adult fellowship training positions increased from 156 to 210, with over 95% fill-rate each year. To leverage the potential for positive change in wake of the 2015 study, authors note that creative strategies for the retention of international medical graduates and new entrants into the rheumatology workforce are warranted.
The authors also highlight how financial incentive programs, which offer scholarships, loans with service requirements and loan repayment or forgiveness, may aid rheumatology. They write, “Expanding financial incentives with service requirements may increase access to care in rural and underserved communities. Surveys suggest that competitive salaries, professional development, knowledgeable support staff and professional support increase the likelihood of provider retention in rural or underserved areas after completion of service commitments.”
The authors also note that since the 2005 study, “nurse practitioners and physician assistants have been shown to be quite effective in managing treat-to-target goals in a rheumatology practice.” They encourage the further exploration into recruitment and training strategies that enable nurse practitioners and physician assistants to be included into the adult rheumatology workforce.
“The ACR/ARHP is committed to optimizing quality rheumatology care and facilitating access to rheumatology care,” conclude the authors. “This will require a passionate vision and innovative strategies by the ACR/ARHP, as well as at the state and federal levels … Decreasing insurance barriers and healthcare regulations may allow more rapid, timely, and creative solutions to offset the projected rheumatologist shortage and the maldistribution of rheumatologists in the U.S.”
Battafarano DF, Ditmyer M, Bolster MB, et al. 2015 American College of Rheumatology Workforce study: Supply and demand projections of adult rheumatology workforce, 2015–2030. Arthritis Care Res (Hoboken). 2018 Apr;70(4):617–626. doi: 10.1002/acr.23518.