When treating patients with steroids, the recommended starting dose is 20–40 mg prednisone daily.2 If there is a response over the next one to three months, the dose should be tapered to 5–15 mg daily and then continued for nine to 12 months.2 The presence of irreversible Stage IV fibrotic disease is a potential reason that a patient may not respond to steroids, because these patients may not have active inflammation for which steroids can be effective.3
It should be noted that this patient had highly advanced Stage IV disease and had been treated with high-dose prednisone for over three months at the time of his massive hemoptysis. In addition, pulmonary hypertension is commonly seen in Stage IV sarcoidosis, and steroids have not been shown to result in a significant hemodynamic response in this subset of patients. Thus, the role of steroids in advanced Stage IV disease is limited.4
Given the potential adverse effects of their chronic use, frequent clinical reassessments should be made to evaluate the continued need for and appropriate dosage of steroids in pulmonary sarcoidosis. In addition to the well-known effects on bone health and the endocrine system, steroids increase the risks of opportunistic infections that can be life threatening.
When patients with pulmonary sarcoidosis who are being treated with steroids develop clinical changes, such as hemoptysis, a low threshold for imaging is required. The estimated incidence of chronic cavitary aspergillosis in sarcoidosis is 2%, and hemoptysis is an important complication of this infection, which can present with a wide range of signs and symptoms.5
Hemoptysis is thought to arise from local vascular invasion by the Aspergillus organism, and it can result in life-threatening bleeding, as seen in this patient. Itraconazole, voriconazole and even intracavitary amphotericin B and voriconazole have been used to treat aspergillomas, but the treatment of these infections in sarcoidosis is not well established.4
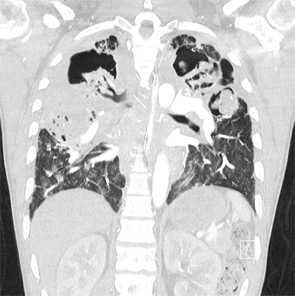
A coronal CT view demonstrating right and left upper lobe mycetomas.
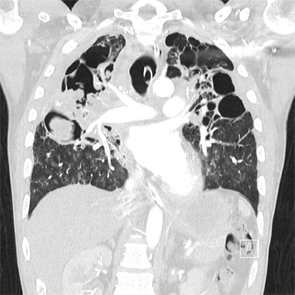
A coronal CT view demonstrating right upper and middle lobe mycetomas.
Conclusion
The potential role and appropriate dosage of corticosteroids should be carefully evaluated in patients with pulmonary sarcoidosis. These patients should be monitored for changes in symptoms, including worsening cough, hemoptysis and dyspnea, because these may imply worsening sarcoidosis, but they should also be evaluated thoroughly to rule out infection, malignancy or worsening pulmonary hypertension. Steroids carry significant and potentially life-threatening risks and are not warranted in all patients with this disease.


