(Click for larger image)
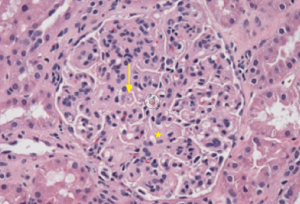
Figure 1: Hematoxylin & Eosin Staining
Enlarged, hypercellular and lobular-appearing glomeruli; capillary loops are thickened and poorly defined (arrow). The mesangium is moderately expanded by extracellular matrix and increased numbers of mononuclear cells (star).
A 35-year-old female with a history of systemic lupus erythematosus (SLE) without kidney involvement was admitted to our hospital with low-grade fevers, headache, increasing lower extremity edema and elevated blood pressure.
History
She was first diagnosed with SLE as a teenager when she developed oral ulcers and pleuritic chest pain and tested positive for anti-Smith and anti-nuclear antibodies (ANAs), meeting four of 11 ACR criteria for SLE. As an adult, her SLE recurred every few years, manifesting as oral ulcers, alopecia, arthritis, biopsy-proven leukocytoclastic vasculitis (LCV) over her lower extremities and hypocomplementemia. She had no prior episodes of nephritis.
Until two months prior to presentation, her symptoms were well controlled with hydroxychloroquine, mycophenolate mofetil (MMF) and low-dose prednisone. However, while transitioning between rheumatologists, she stopped her medications and developed her usual SLE symptoms, including oral ulcers, arthritis and lower extremity rash. In addition, she reported low-grade fevers, headaches, fatigue, pleuritic chest pain, dyspnea on exertion, six-pillow orthopnea and pitting edema in her lower extremities. A physician family member prescribed 60 mg of prednisone daily. Her breathing and chest pain improved, but she continued to experience headaches and recorded her own blood pressures, which reached systolic blood pressure of 225 mmHg.
Her new rheumatologist found hypocomplementemia and proteinuria, hydroxychloroquine was resumed, MMF changed to azathioprine, and lisinopril was prescribed. Over the next several weeks, her symptoms improved, but hypocomplementemia and proteinuria continued. Her nephrologist scheduled an elective kidney biopsy, but prior to her biopsy low-grade fevers, headache, pitting edema and hypertension recurred. She sought emergency care resulting in admission to our institution.
Hospital Assessment
On initial assessment, she was afebrile with a blood pressure of 170/90 mmHg, breathing comfortably with an oxygen saturation of 97% on room air. She was in no distress and had moderate periorbital edema. Her lungs were clear to auscultation. Examination of her lower extremities revealed synovitis in her left ankle and bilateral lower extremity pitting edema with an overlying palpable purpuric rash with a few shallow ulcers.
Her basic metabolic profile was within normal limits and included a BUN of 22 mg/dL and creatinine of 0.83 mg/dL. Her complete blood cell count was remarkable for a low, but stable hematocrit at 27% (lower limit of normal 36%). ESR and CRP were elevated at 27 mm/hr and 4.4 mg/L, respectively. Serologies yielded a positive ANA at 1:640 (speckled), while the remainder of the extractable nuclear and double-stranded DNA autoantibodies was negative. Complement levels were low, with C3 at 52 and C4 at 2 mg/dL, respectively (normal C3 90–180, C4 10–40 mg/dL). Her urine contained 3+ blood, 3+ protein and hyaline casts. The spot urine protein to creatinine ratio was 328:51, suggesting 6.4 g of urinary protein excretion over 24 hours. Antiphospholipid antibodies were negative, while ANCA and cryoglobulins were pending.


