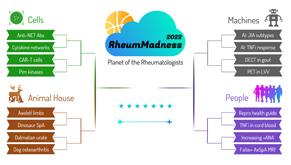
 Editor’s note: RheumMadness is the place for everyone crazy about rheumatology to connect, collaborate, compete and learn together. During RheumMadness, rheumatology concepts represent teams that compete against each other in a tournament, much like basketball teams do in the NCAA’s March Madness tournament. In a series for The Rheumatologist, readers will get a chance to read the scouting reports for each concept team. These reports are written by rheumatology fellows from 13 programs throughout the U.S.
Editor’s note: RheumMadness is the place for everyone crazy about rheumatology to connect, collaborate, compete and learn together. During RheumMadness, rheumatology concepts represent teams that compete against each other in a tournament, much like basketball teams do in the NCAA’s March Madness tournament. In a series for The Rheumatologist, readers will get a chance to read the scouting reports for each concept team. These reports are written by rheumatology fellows from 13 programs throughout the U.S.
Don’t forget to submit your RheumMadness 2022 bracket by March 25. The more your picks match those of our Blue Ribbon Panel of rheumatologists, the more points you get. Learn more about the panel and how the brackets work online.
Connect with RheumMadness by subscribing to the podcast and joining the conversation on Twitter, #RheumMadness. Learn more on the RheumMadness website.
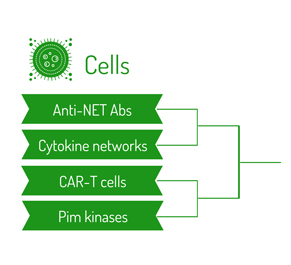
Region: Cells Team: CAR-T Cells
Chimeric antigen receptor T (CAR-T) cells are made by combining T cell receptor constant variant domains and antibody variable domains. Anti-CD19-targeted CAR-T cells have been shown to be a power forward in the destruction of B cell malignancies, even in patients boxed out of other therapies.
Inspired by this success with CAR-T cell therapy in hematologic malignancies, CD19 CAR-T cell therapy is actively being recruited as the next MVP for B cell depletion therapy in patients with autoimmune disease. It’s hypothesized this elite therapy can better access—within lymphatic organs and inflamed tissues for example—and persistently deplete autoreactive B cells than current players, such as rituximab.
 Given that CD19 is expressed during all major states of B cell maturation, it’s speculated that anti-CD19 therapy may lead to depletion of pro-B cell plasmablasts secreting pathologic autoantibodies and some plasma cells. A case report by Mougiakakos et al. in which a severe case of refractory systemic lupus erythematosus (SLE) was swiftly knocked out by CD19 CAR-T cell therapy illustrates the immense power of this emerging, immunosuppressive all-star in the treatment of rheumatic diseases.1
Given that CD19 is expressed during all major states of B cell maturation, it’s speculated that anti-CD19 therapy may lead to depletion of pro-B cell plasmablasts secreting pathologic autoantibodies and some plasma cells. A case report by Mougiakakos et al. in which a severe case of refractory systemic lupus erythematosus (SLE) was swiftly knocked out by CD19 CAR-T cell therapy illustrates the immense power of this emerging, immunosuppressive all-star in the treatment of rheumatic diseases.1
CAR-T cell therapies have been tested in mouse models for type 1 diabetes, lupus, multiple sclerosis, colitis and other diseases with at least some measurable benefit. Additionally, pre-clinical CAR-T studies have been completed or are ongoing for rheumatoid arthritis (RA), SLE and systemic sclerosis. Other potential applications include CAR-T cells expressing citrullinated antigens to target anti-citrulline B cells to treat RA and CAR-T reg cell therapies.2
Implications
CAR-T cells represent a major shift in the nature of therapeutics for rheumatology—possibly more profound than the addition of biologic disease-modifying anti-rheumatic drugs (DMARDs) to the conventional synthetic DMARD playbook in the late 1990s and early 2000s.
These treatments are not just a different type of molecule; they are a cell-based therapy. They have the potential for extreme specificity—both in terms of disease/antigen specificity and patient specificity—because they use autologous T cells. This player-to-player defense may dramatically lower the personal fouls associated with the treatment of rheumatic diseases. Their theoretical ability to target fibroblast populations may also lead to breakthroughs in treating patients with fibrosing disorders, including but not limited to interstitial lung disease and systemic sclerosis, for which current therapeutic options are limited.
The prospect of using CAR-T cells for the treatment of rheumatic diseases raises several exciting questions. Will this therapeutic potential dramatically accelerate antigen discovery in the same way monoclonal antibodies spurred our understanding of the role of cytokines/cytokine networks in different diseases and facilitate clinicopathologic correlation between these antigens and disease phenotype? How can CAR-T cell therapy team up with other therapies, such as conventional synthetic and/or biologic DMARDs? Will adverse effects, such as the risk of cytokine release syndrome or immunosuppression, prove intolerable to patients with rheumatic diseases? Other questions, such as how this technology will change the landscape of insurance approval if adopted across the league, are more technical but perhaps equally important.
Chances in the Tournament
Due to its novelty and marked potential for clinical impact in the near future, the CAR-T Cells team will likely be a crowd favorite in RheumMadness 2022. CAR-T cells could lead to a paradigm shift in the treatment of rheumatic diseases, running a fast-break beyond cytokine- and antimetabolite-based treatment regimens and making a lay-up toward a therapy that selectively targets and slam dunks disease-causing cells while sparing others.
Although the first-round opponent, Pim Kinases, also represents a therapeutic target in oncology that may be repurposed in rheumatology, CAR-T cells are more unlike our current therapies, have a broader role in oncology treatment than Pim kinase inhibitors and have been shown to be a game-winning play in a patient with severe, refractory SLE. And let’s face it—CAR-T cells are cool and exactly the type of topic that excites rheumatologists.
We believe the Blue Ribbon Panel will appreciate this innovative treatment, even in comparison with the other, better-known categories in the Cells Region. Whether CAR-T Cells will beat some of the more immediately, clinically relevant topics in the Machines and People regions will depend on how the panel weighs the time it will take for CAR-T cells to reach clinical use. With the potential to treat so many of our diseases in which current therapeutic options remain inadequate, CAR-T cells is a worthy competitor against any other team in this year’s bracket.
Guy Katz, MD, is a second-year rheumatology fellow at Massachusetts General Hospital, Boston.
Ian Cooley, MD, is a second-year rheumatology fellow at Massachusetts General Hospital, Boston.
Duncan Moore, MD, is a second-year rheumatology fellow at Massachusetts General Hospital, Boston.
Jacquelyn Nestor, MD, PhD, is a first-year rheumatology fellow at Massachusetts General Hospital, Boston.
Steven Witte, MD, PhD, is a first-year rheumatology fellow at Massachusetts General Hospital, Boston.
References
- Mougiakakos D, Krönke G, Völkl S, et al. CD19-targeted CAR T cells in refractory systemic lupus erythematosus. N Engl J Med. 2021 Aug 5;385(6):567–569.
- Orvain C, Boulch M, Bousso P, et al. Is there a place for chimeric antigen receptor T cells in the treatment of chronic autoimmune rheumatic diseases. Arthritis Rheumatol. 2021 Nov;73(11):1954–1965.
 Experience All of RheumMadness
Experience All of RheumMadness
During RheumMadness, rheumatology concepts represent teams that compete against each other in a tournament, much like basketball teams do in the NCAA’s March Madness tournament. In a series for The Rheumatologist, readers will get a chance to read the scouting reports. Check out the reports from each region:
Region: Cells
Region: Animal House
Region: Machines
Region: People
• False Positive MRI in Axial SpA
Don’t forget to submit your RheumMadness 2022 bracket by March 25. The winner of each match-up is decided by a seven-member Blue Ribbon Panel of rheumatologists. The panel will vote based on which topic they think is most important to patients, providers and researchers—both now and in the future. The more your picks match those of the panel, the more points you get. The tournament results will be released in four rounds from March 26–April 4. Prizes will be given to participants with the top scores in the following categories: 1) attending/APP, 2) fellow and 3) resident/medical student. The prize is a custom RheumMadness coffee mug and a lifetime of bragging rights.
Connect with RheumMadness by subscribing to the podcast and joining the conversation on Twitter, #RheumMadness. Learn on the RheumMadness website.



