Two key themes for workforce solutions are to train providers for rheumatology care and to sustain the rheumatology healthcare team. “Achieving our long-term goals,” says Dr. Battafarano, “requires a community investment in rheumatology care and the workforce. The rheumatology needs and attributes of a community can enable financial incentive programs, loan repayment options, financial support for telemedicine, and end-of-career stepdown strategies, among other ideas.”
Given the shortage of adult and pediatric rheumatologists throughout the U.S., the Workforce Solutions Committee will initially focus on implementing interventions in communities identified as both having a shortage of rheumatology providers and with attributes that may enhance the sustainability of rheumatology care.
Workforce Interventions
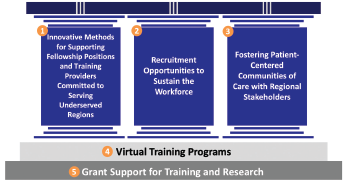
Figure 1: Workforce Interventions. The three pillars represent interventions focused on training the rising provider workforce, sustaining the presence of existing providers, and forging relationships with stakeholders that can influence patient centered care. These pillars are supported by the ongoing work of the ACR related to virtual training programs and grant funding.
The workforce initiative will focus on five core interventions: three primary pillars (see Figure 1) to enhance the workforce and two critical foundations to support these interventions. These pillars include training providers committed to serving in underserved areas, sustaining the presence of these providers in these areas, and partnering with regional stakeholders to foster patient-centered communities. These three pillars are supported by the increased use of virtual training programs and grants for training and research.
Addressing only one pillar is not enough. “The ACR has traditionally focused on training more rheumatology fellows to increase the overall number of rheumatologists in the U.S.,” says Dr. Battafarano. “We realize now that we need to implement change in a variety of areas.” Among the areas Dr. Battafarano cited are partnering with ACGME to creatively introduce fellowships in underserved areas, augmenting the rheumatology healthcare team in underserved areas with primary care physicians (PCPs) and APPs, finding creative ways to ensure recruitment and retention of the current workforce, and partnering with payers to incentivize rheumatologists to work in underserved areas.
Training
Starting with the first pillar and expanding ACGME fellowship initiatives, the workforce solutions group is working on increasing the number of fellowship training slots in geographically underserved areas by developing new training programs within those areas and by bringing training to the communities via collaborations with established programs in adjacent areas, and expanding access via telemedicine or virtual training.
Example: Seattle Children’s Hospital is training a pediatric rheumatology fellow who plans to practice in Montana, a state without a pediatric rheumatologist. The fellow will work as a solo practitioner in Montana, but will be supported by colleagues at the Children’s Hospital of Seattle by sharing overnight phone calls, and having a referral base for more complicated patients.
Beth Jonas, MD, a member of the Workforce Solutions Committee, notes that despite the popularity of adult rheumatology among internal medicine trainees, there are too few fellowship slots to train them. In 2019–20, for example, of 335 applicants for adult rheumatology fellowships, only 242 were matched—leaving 94 applicants who did not match. In 2020–21, 84 applicants did not match. The workforce study group estimates a 34% increase in training slots is required by 2030 to meet demand.
“Although almost any area of the country could use more training slots, we are focused on building training capacity in the most underserved areas, including the Northwest, South Central and Southwest,” says Dr. Jonas. “That is important because we know trainees will often stay and practice in the community or state where they grew up or in the community or state in which they did their training.
“Bringing rheumatology training to underserved areas will begin to build rheumatology communities of care where they do not currently exist,” she adds.
‘The workforce shortage is an existential threat to the field of rheumatology & to the care we deliver to our patients.’ —ACR President Kenneth Saag, MD
For pediatric rheumatology, the numbers are even more stark: An estimated 142% increase in training slots will be needed by 2030 to meet demand. Unlike adult rheumatology fellowships, however, the challenge for pediatric rheumatology fellowships is to increase demand for them. Only a small number of pediatric fellowship positions are available nationwide, and most are clustered in urban areas given the need for pediatric rheumatologists to work in a children’s hospital with other pediatric specialists to care for their patients. A pediatric rheumatologist faces more challenges than adult rheumatologists working alone in a rural community.
“Therefore, if we plan to open more pediatric fellowship slots, we are working to strategically open them in resource-limited settings where there is a medical school and a general pediatrics residency program but no fellowship program,” says Colleen K. Correll, MD, MPH, chair of the Pediatric Rheumatology Special Committee, and a member of the Workforce Solutions Committee.