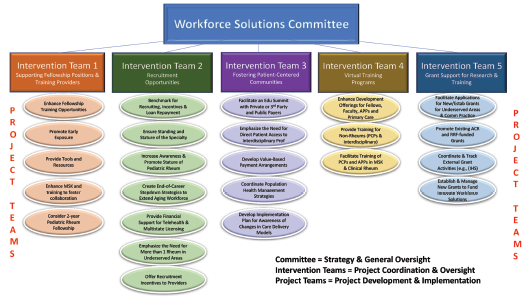
Figure 2: The Projects
For both the adult and pediatric rheumatology workforce, another strategy to increase the supply of rheumatology providers is to train members of the entire healthcare team—PCPs, nurse practitioners (NPs), physician assistants (PAs), physical therapists and occupational therapists—to provide care for patients with rheumatic illnesses. According to Dr. Jonas, the ACR already has a successful training program (The Training Rheum) offered to NPs and PAs via an online curriculum and in clinical face-to-face settings, and she anticipates the development of similar training programs that target PCPs and other members of the healthcare team.
An additional strategy may be to promote early exposure to rheumatology to broaden the applicant pool, by offering additional musculoskeletal training in medical school or core residency programs, or by offering mentorship programs within specialty-specific interest groups at medical schools in underserved regions.
Recruitment
The second pillar includes innovative recruitment models for the rheumatology workforce in underserved areas. This would include such projects as redefining conversations with recruiters to increase awareness of adult rheumatology and promote the stature of pediatric rheumatology, benchmarking for recruiting and offering compensation incentives, and creating end-of-career stepdown strategies that could extend an established rheumatologist’s career.
Collaboration
The third pillar recognizes the need to collaborate with regional partners to foster patient-centered communities. This could include partnering with regional health plans and insurance providers (e.g., provider-sponsored and/or self-insurance health plans, Medicaid plans for pediatric populations and Medicare Advantage plans), developing value-based payment arrangements for rheumatic care, and/or coordinating population health management strategies. When possible, it could include direct patient access for interdisciplinary professionals like physical therapy and occupational therapy.

Dr. Jonas
The two foundations supporting the three pillars are ACR Virtual Training Programs and grants for both training and research primarily supported by the Rheumatology Research Foundation. The virtual training opportunities and experience for fellowship training nationwide provided by the ACR during the pandemic can be readily applied to further virtual training of PCPs, APPs, and interdisciplinary specialties. The Foundation will enable grant support for training but also research grants to support collaborative health services research, quality outcome measures and more.
To successfully identify and implement the proposed interventions, the ACR recognized a need to partner with an experienced consultant to assist in collaborating with local and regional healthcare markets and who understood the challenges of the workforce. The Committee chose a workforce management consultant who did a thorough assessment of the national workforce.
“Our workforce consultant has analyzed every region of the U.S., assessing rheumatologist distribution, provider supply attributes, population attributes including cost of living and quality of life, and the payer landscape for providers, hospitals, and supply of primary care providers to determine the areas of most need for rheumatology care,” says Dr. Battafarano.
Based on this assessment, the consultant and the ACR work group identified three main regions in the U.S.—Northwest, South Central and Southwest—to implement pilot intervention programs for enhancing the rheumatologic workforce in those areas. The potential interventions are listed in Figure 2.
Implementation & Benchmarks
Implementation of workforce solution initiatives will occur in two phases. Phase 1 is well underway. This phase involves defining and prioritizing projects to meet the pre-defined benchmarks and timelines.
Pilot programs in the three regions identified above will then be launched. Within each region, potential partners will be identified, recruitment incentives defined and blueprints of prioritized programs implemented.
Phase 2 will involve scaling up these efforts by replicating one or more of the pilot programs in different locations and advancing additional opportunities defined by successful pilot programs.
Critical benchmarks will include access to care, total training for primary care providers, impact of training, number of rheumatologists and rheumatology care providers, impact of telemedicine and downstream benefits of rheumatology care in the community.
Dr. Saag emphasizes that the ACR will provide dedicated resources to increasing the rheumatology workforce and its better distribution and increased diversity. “These are the things we value as a college,” he says. “Some of these are longer term goals, and we may not see all of these [improvements] right away, but over time.”
Mary Beth Nierengarten is a freelance medical journalist based in Minneapolis.


