Rawpixel.com / shutterstock.com
The growing rheumatologist workforce shortage has loomed over the profession, threatening to undercut the delivery of care to the increasing number of patients with rheumatic conditions.
“The workforce shortage is an existential threat to the field of rheumatology and to the care we deliver to our patients,” says ACR President Kenneth Saag, MD, who lauded the efforts of the newly formed ACR Workforce Solutions Committee to “crucially and creatively” tackle an issue that has remained inadequately addressed for too long (see sidebar).
The significance of the workforce shortage in rheumatology was documented in a 2015 workforce study that assessed the supply and demand of the adult rheumatology workforce up to 2030.1 “Its findings were sobering,” says Daniel F. Battafarano, DO, chair of the ACR Workforce Solutions Committee, and lead author of the study. By 2030, the number of rheumatologists was projected to drop by 25% from 2015 baseline levels while the patient demand for rheumatologic care is projected to exceed the supply of rheumatologists by over 100%. “For the most part, we have seen a trend for these numbers becoming a reality,” he says.
A critical finding in the workforce study was the geographic maldistribution of adult rheumatologists across the U.S., with strong representation in the major urban and suburban areas in the Northeast, West Coast and Mid-Atlantic states, and poor representation in other geographic areas, particularly rural and underserved areas.
For pediatric rheumatologists, the projection is even more dire. Data show the current scarcity of pediatric rheumatologists across the U.S. will worsen significantly by 2030, with demand for pediatric rheumatology services exceeding twice the supply.2 Severe shortages of pediatric rheumatology providers were noted in all geographic areas.
In October 2021, the ACR Board of Directors approved a three-year workforce plan developed by the Workforce Solutions Committee that will address five areas of workforce intervention:
- Increasing fellowships;
- Promoting adult and pediatric rheumatology;
- Forming partnerships in managed care;
- Creating virtual training for primary care physicians (PCPs) and advanced practice providers (APPs); and
- Developing grants and awards to support workforce growth.
The recommended projects within each intervention area will focus on regions with a limited number of rheumatologists but that are supported by a range of community assets. These include a strong pipeline of medical schools and resident programs, a patient population that can support a full-time rheumatologist, not-for-profit hospitals open to supporting trainees, and legislation that permits APPs to provide patient care for rheumatic diseases.
The following describes the innovative approach to enhancing the rheumatology workforce in underserved areas proposed by the Workforce Solutions Committee.
Train & Sustain
Two key themes for workforce solutions are to train providers for rheumatology care and to sustain the rheumatology healthcare team. “Achieving our long-term goals,” says Dr. Battafarano, “requires a community investment in rheumatology care and the workforce. The rheumatology needs and attributes of a community can enable financial incentive programs, loan repayment options, financial support for telemedicine, and end-of-career stepdown strategies, among other ideas.”
Given the shortage of adult and pediatric rheumatologists throughout the U.S., the Workforce Solutions Committee will initially focus on implementing interventions in communities identified as both having a shortage of rheumatology providers and with attributes that may enhance the sustainability of rheumatology care.
Workforce Interventions
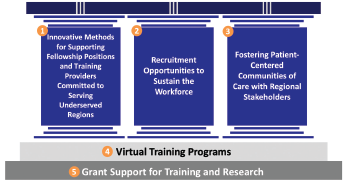
Figure 1: Workforce Interventions. The three pillars represent interventions focused on training the rising provider workforce, sustaining the presence of existing providers, and forging relationships with stakeholders that can influence patient centered care. These pillars are supported by the ongoing work of the ACR related to virtual training programs and grant funding.
The workforce initiative will focus on five core interventions: three primary pillars (see Figure 1) to enhance the workforce and two critical foundations to support these interventions. These pillars include training providers committed to serving in underserved areas, sustaining the presence of these providers in these areas, and partnering with regional stakeholders to foster patient-centered communities. These three pillars are supported by the increased use of virtual training programs and grants for training and research.
Addressing only one pillar is not enough. “The ACR has traditionally focused on training more rheumatology fellows to increase the overall number of rheumatologists in the U.S.,” says Dr. Battafarano. “We realize now that we need to implement change in a variety of areas.” Among the areas Dr. Battafarano cited are partnering with ACGME to creatively introduce fellowships in underserved areas, augmenting the rheumatology healthcare team in underserved areas with primary care physicians (PCPs) and APPs, finding creative ways to ensure recruitment and retention of the current workforce, and partnering with payers to incentivize rheumatologists to work in underserved areas.
Training
Starting with the first pillar and expanding ACGME fellowship initiatives, the workforce solutions group is working on increasing the number of fellowship training slots in geographically underserved areas by developing new training programs within those areas and by bringing training to the communities via collaborations with established programs in adjacent areas, and expanding access via telemedicine or virtual training.
Example: Seattle Children’s Hospital is training a pediatric rheumatology fellow who plans to practice in Montana, a state without a pediatric rheumatologist. The fellow will work as a solo practitioner in Montana, but will be supported by colleagues at the Children’s Hospital of Seattle by sharing overnight phone calls, and having a referral base for more complicated patients.
Beth Jonas, MD, a member of the Workforce Solutions Committee, notes that despite the popularity of adult rheumatology among internal medicine trainees, there are too few fellowship slots to train them. In 2019–20, for example, of 335 applicants for adult rheumatology fellowships, only 242 were matched—leaving 94 applicants who did not match. In 2020–21, 84 applicants did not match. The workforce study group estimates a 34% increase in training slots is required by 2030 to meet demand.
“Although almost any area of the country could use more training slots, we are focused on building training capacity in the most underserved areas, including the Northwest, South Central and Southwest,” says Dr. Jonas. “That is important because we know trainees will often stay and practice in the community or state where they grew up or in the community or state in which they did their training.
“Bringing rheumatology training to underserved areas will begin to build rheumatology communities of care where they do not currently exist,” she adds.
‘The workforce shortage is an existential threat to the field of rheumatology & to the care we deliver to our patients.’ —ACR President Kenneth Saag, MD
For pediatric rheumatology, the numbers are even more stark: An estimated 142% increase in training slots will be needed by 2030 to meet demand. Unlike adult rheumatology fellowships, however, the challenge for pediatric rheumatology fellowships is to increase demand for them. Only a small number of pediatric fellowship positions are available nationwide, and most are clustered in urban areas given the need for pediatric rheumatologists to work in a children’s hospital with other pediatric specialists to care for their patients. A pediatric rheumatologist faces more challenges than adult rheumatologists working alone in a rural community.
“Therefore, if we plan to open more pediatric fellowship slots, we are working to strategically open them in resource-limited settings where there is a medical school and a general pediatrics residency program but no fellowship program,” says Colleen K. Correll, MD, MPH, chair of the Pediatric Rheumatology Special Committee, and a member of the Workforce Solutions Committee.
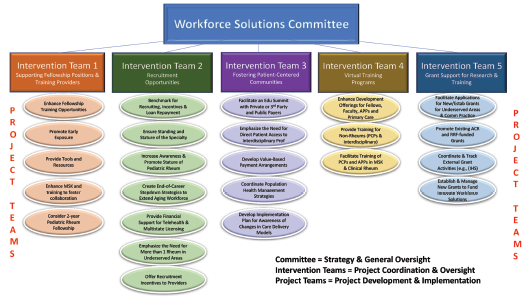
Figure 2: The Projects
For both the adult and pediatric rheumatology workforce, another strategy to increase the supply of rheumatology providers is to train members of the entire healthcare team—PCPs, nurse practitioners (NPs), physician assistants (PAs), physical therapists and occupational therapists—to provide care for patients with rheumatic illnesses. According to Dr. Jonas, the ACR already has a successful training program (The Training Rheum) offered to NPs and PAs via an online curriculum and in clinical face-to-face settings, and she anticipates the development of similar training programs that target PCPs and other members of the healthcare team.
An additional strategy may be to promote early exposure to rheumatology to broaden the applicant pool, by offering additional musculoskeletal training in medical school or core residency programs, or by offering mentorship programs within specialty-specific interest groups at medical schools in underserved regions.
Recruitment
The second pillar includes innovative recruitment models for the rheumatology workforce in underserved areas. This would include such projects as redefining conversations with recruiters to increase awareness of adult rheumatology and promote the stature of pediatric rheumatology, benchmarking for recruiting and offering compensation incentives, and creating end-of-career stepdown strategies that could extend an established rheumatologist’s career.
Collaboration
The third pillar recognizes the need to collaborate with regional partners to foster patient-centered communities. This could include partnering with regional health plans and insurance providers (e.g., provider-sponsored and/or self-insurance health plans, Medicaid plans for pediatric populations and Medicare Advantage plans), developing value-based payment arrangements for rheumatic care, and/or coordinating population health management strategies. When possible, it could include direct patient access for interdisciplinary professionals like physical therapy and occupational therapy.

Dr. Jonas
The two foundations supporting the three pillars are ACR Virtual Training Programs and grants for both training and research primarily supported by the Rheumatology Research Foundation. The virtual training opportunities and experience for fellowship training nationwide provided by the ACR during the pandemic can be readily applied to further virtual training of PCPs, APPs, and interdisciplinary specialties. The Foundation will enable grant support for training but also research grants to support collaborative health services research, quality outcome measures and more.
To successfully identify and implement the proposed interventions, the ACR recognized a need to partner with an experienced consultant to assist in collaborating with local and regional healthcare markets and who understood the challenges of the workforce. The Committee chose a workforce management consultant who did a thorough assessment of the national workforce.
“Our workforce consultant has analyzed every region of the U.S., assessing rheumatologist distribution, provider supply attributes, population attributes including cost of living and quality of life, and the payer landscape for providers, hospitals, and supply of primary care providers to determine the areas of most need for rheumatology care,” says Dr. Battafarano.
Based on this assessment, the consultant and the ACR work group identified three main regions in the U.S.—Northwest, South Central and Southwest—to implement pilot intervention programs for enhancing the rheumatologic workforce in those areas. The potential interventions are listed in Figure 2.
Implementation & Benchmarks
Implementation of workforce solution initiatives will occur in two phases. Phase 1 is well underway. This phase involves defining and prioritizing projects to meet the pre-defined benchmarks and timelines.
Pilot programs in the three regions identified above will then be launched. Within each region, potential partners will be identified, recruitment incentives defined and blueprints of prioritized programs implemented.
Phase 2 will involve scaling up these efforts by replicating one or more of the pilot programs in different locations and advancing additional opportunities defined by successful pilot programs.
Critical benchmarks will include access to care, total training for primary care providers, impact of training, number of rheumatologists and rheumatology care providers, impact of telemedicine and downstream benefits of rheumatology care in the community.
Dr. Saag emphasizes that the ACR will provide dedicated resources to increasing the rheumatology workforce and its better distribution and increased diversity. “These are the things we value as a college,” he says. “Some of these are longer term goals, and we may not see all of these [improvements] right away, but over time.”
Mary Beth Nierengarten is a freelance medical journalist based in Minneapolis.
The Mission
The mission of the Workforce Solutions Committee is to innovate and implement workforce solutions to broaden and sustain high-quality adult and pediatric rheumatology care in underserved communities while partnering with local stakeholders. To that end, the workforce solution initiatives will focus on finding regional workforce solutions to address the lack of rheumatology providers in underserved areas.
References
- Battafarano DF, Ditmyer M, Bolster MB, et al. 2015 American College of Rheumatology workforce study: Supply and demand projections of adult rheumatology workforce, 2015-2030. Arthritis Care Res. 2018;70(4):617–626.
- Correll CK, Ditmyer MM, Mehta J, et al. 2015 American College of Rheumatology workforce study and demand projections of pediatric rheumatology workforce, 2015–2030. Arthritis Care Res. 2022;74(3):340–348.