Major relevant examples include proposals to rein in high drug prices for patients, a goal the ACR shares with policymakers and others. The ACR strongly believes that safe and effective treatments should be available to patients at the lowest possible cost. Unfortunately, many of the efforts by payers to lower drug expenses result in reduced access to effective and affordable treatments for patients that need them. The College has put forward a number of proposed policies that would bring down drug costs for patients while protecting patient access to treatments. These include:
- Requiring plans to apply a substantial portion of rebates at the point of sale;
- Establishing a beneficiary out-of-pocket maximum in the Medicare Part D catastrophic phase to provide beneficiaries with better protection against high drug costs;
- Decreasing concentration in the pharmacy benefit manager (PBM) market and other segments of the supply chain;
- Increasing transparency in how pharmaceutical companies, pharmacy benefit managers and health insurance companies determine the cost of prescription medications;
- Increasing transparency of any incentives given by drug companies to pharmacy benefit managers or health insurance companies related to the dispensing or promotion of their manufactured drugs;
- Eliminating excessive patient cost sharing usually required by formularies’ specialty tiers or providing an expeditious exception and appeal process for Part D beneficiaries who are affected by specialty tier practices; and
- Allowing Medicare to negotiate with pharmaceutical companies to achieve more affordable drug pricing.
Trump’s Plan
In May, the U.S. Department of Health and Human Services (HHS) released a request for information (RFI) related to the Trump administration’s blueprint to lower drug prices and reduce patients’ out-of-pocket costs. The ACR agrees that action on high drug prices is long overdue, and we were pleased to see the inclusion of proposals that would create PBM pricing transparency, promote biosimilar development and reduce out-of-pocket costs in Part D. However, we were concerned that several proposals—particularly allowing Part D plans to further restrict drug formularies and moving Part B drugs into Part D—could make it more difficult for our patients to access needed therapies. The ACR is closely analyzing these proposals as we develop a comprehensive response to the RFI ahead of the July deadline for comments.
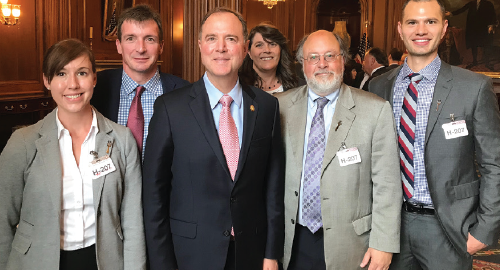
ACR President David Daikh, MD, PhD, with
Rep. Adam Schiff (D-CA-28) and California rheumatology advocates. From left: Christina Downey, MD; William Robinson, MD, PhD; Rep. Schiff; ARHP President Sandra Mintz, MSN, RN; Dr. Daikh; and Matthew Baker, MD.


