GraphicsRF / shutterstock.com
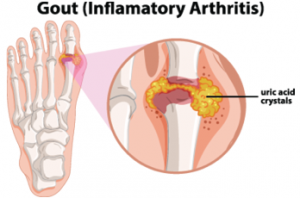
SNOWMASS VILLAGE, COLO.—The 2019 ACR Winter Rheumatology Symposium featured a session on gout. Despite a good understanding of its pathogenesis and the many effective therapies to treat it, gout remains a major public health problem in the U.S. Ann K. Rosenthal, MD, Will and Cava Ross professor of medicine and chief of the Division of Rheumatology at the Medical College of Wisconsin, Milwaukee, says that of the estimated 8–10 million people affected by gout, only 3.1 million are on urate-lowering therapy, and only 40% of people treated with allopurinol are receiving adequate doses to achieve target uric acid levels.1
Misdiagnosis at the point of care, leading to under- and overdiagnosis, and a lack of patient compliance with prescribed, effective treatments, are major obstacles to effective gout management.
ACR & EULAR Guidelines
One way to remedy mismanagement, said Dr. Rosenthal, is for rheumatologists to consider adopting the treatment suggestions in the most recent ACR and European League Against Rheumatism (EULAR) gout guideline papers.1,2
These guidelines focus on the need to manage gout to achieve target uric acid levels. They also incorporate recent evidence-based support for what Dr. Rosenthal calls the “random and dogmatic” gout treatment approaches used in the past.
Both guidelines provide support for the appropriate use of anti-inflammatory prophylactic drugs when starting and changing uric acid-lowering agents. [Note: The ACR is currently updating its gout guideline, with anticipated publication by early 2020.]
Given the lack of good management of gout at the point of care, Dr. Rosenthal also emphasized using the guidelines “to help educate the community of non-rheumatologists who are often the first medical contacts for gout patients.”
The most recent ACR & EULAR gout guideline papers focus on the need to manage gout to achieve target uric acid levels.
Controversies in Treatment
Dr. Rosenthal touched on issues related to uric acid that remain under debate. One main issue she discussed is the lack of full understanding of the benefits of treating high uric acid levels, which can prevent or reduce chronic kidney disease (CKD) in people who are at increased risk of end-stage renal disease.

Dr. Rosenthal
Dr. Rosenthal touched on the complex role of uric acid in health and disease, and the incomplete understanding of the consequences of manipulating levels of uric acid in patients at risk of developing CKD, by highlighting data from a meta-analysis of 16 trials that looked at the effects of uric-lowering therapy on kidney outcomes in patients with CKD.3
Results of the pooled analysis showed a potential modest benefit of uric acid-lowering drugs in delaying progression of CKD, as shown by improvement in kidney outcomes (i.e., kidney failure events, proteinuria and the rate of change in glomerular filtration rate). Results also showed uric acid-lowering treatment seemed to reduce the risk of cardiovascular events in people with CKD.
Dr. Rosenthal emphasized the conclusion of the study highlighted the limitations of the meta-analysis based on the low quality and heterogeneity of the studies, and the need for higher quality randomized data to provide a more precise understanding of the benefit of uric acid-lowering treatment in this setting.
Dr. Rosenthal pointed to data from another recent study that shed light on the complexity of uric acid levels and their treatment. A study by Cho et al., “U-Shaped Association Between Serum Uric Acid Level and Risk of Mortality: A Cohort Study,” examined the relationship between low and high uric acid levels and the risk of all-cause and cause-specific mortality in a large cohort of men and women (N=375,163). The researchers found a U-shaped link between uric acid levels and adverse outcomes. Specifically, the study found that patients with both high and low uric acid levels had increased all-cause mortality, as well as increased cancer and cardiovascular mortality.4
Given these mixed data on uric acid and the potential consequences of both high and low levels, Dr. Rosenthal ended her talk with a brief discussion on the renewed interest in looking for new treatments for gout, including the development of additional uricosuric agents that reduce the concentration of uric acid in the blood by increasing its excretion in the urine.
Cost of Treatment
Recent controversies around the new uricosuric drug lesinurad, she said, center on disappointing sales revenues. Data show that when combined with a xanthine oxidase inhibitor (XOI), lesinurad reduces uric acid compared to XOI alone. However, this drug carries a high price tag, about $394 per month, compared with other drugs used to treat gout, including allopurinol ($10 per month) and probenecid ($34 per month).
Dr. Rosenthal also mentioned drugs currently in development have both uricosuric and anti-inflammatory properties, which could simplify some of the complicated drug regimens now used to treat gout.
Mary Beth Nierengarten is a freelance medical journalist based in Minneapolis.
References
- Khanna D, FitzGerald JD, Khanna PP, et al. 2012 American College of Rheumatology guidelines for management of gout. Part 1: Systematic nonpharmacologic and pharmacologic therapeutic approaches to hyperuricemia. Arthritis Care Res (Hoboken). 2012 Oct;64(10):1431–1446.
- Richette P, Doherty M, Pascual E, et al. 2016 updated EULAR evidence-based recommendations for the management of gout. Ann Rheum Dis. 2017 Jan;76(1):29–42.
- Su X, Xu B, Yan B, et al. Effects of uric acid-lowering therapy in patients with chronic kidney disease: A meta-analysis. PLoS One. 2017 Nov 2;12(11).
- Cho SK, Chang Y, Kim I, et al. U-shaped association between serum uric acid level and risk of mortality: A cohort study. Arthritis Rheumatol. 2018 Jul;70(7):1122–1132.


