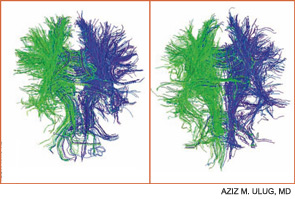
Contemporary techniques for imaging of the brain—MRI, PET, functional MRI, and diffusion tensor imaging (DTI) (see Figures 1 and 2, above)—allow the display of the anatomy of abnormal brain function and the ability to see, literally, thought in action. The images observed by these modalities do not always distinguish functional abnormalities from structural ones; also, demonstrated abnormalities may not correlate closely with cognitive function measured by formal testing. Focal breakdown of the blood–brain barrier may be critical to the localization of brain injury in diseases such as lupus, but intactness of the barrier is not easy to identify by any technology currently applicable to humans. New technologies under investigation may be more successful in defining the blood–brain barrier and may help explain the gap between the presence of autoantibodies in lupus and the occurrence focal brain changes.
Lessons from the Brain
As discussed at the conference, animal models may help define mechanisms of abnormal cognition. Mice that develop clinical lupus or are exposed to lupus autoantibodies (e.g., anti-DNA, antiphospholipid, and anti-NMDA) demonstrate behavioral changes and anatomic abnormalities that parallel those of human lupus. Time-specific disruption of the blood–brain barrier, leukoagglutination, thrombosis, microvascular injury, and autoantibody-mediated cell toxicity are plausible mechanisms of brain injury demonstrable in mice, and sometimes in men.
The Mary Kirkland Center conference’s discussion of animal and human neurobiological, behavioral, and imaging information about cognition concluded that white-matter injury (interfering with brain interconnections) may be more important in lupus than is gray-matter injury, and that immunologically driven brain injury is focal for reasons not yet understood. White-matter damage, particularly in the frontal area, can parallel neuropsychologically defined global deficits of attention and executive function, and is demonstrable on MRI or DTI. Longitudinal studies suggest that cognitive dysfunction in lupus is more likely transient and reversible than permanent.
The Mary Kirkland Center conference led to the following ideas that could inform future research: Due to the wide variability of cognitive symptoms and innate capacities among patients with lupus, longitudinal study of small numbers of individual patients may be more informative than cross-sectional studies of large patient groups. Because patients’ descriptions of cognitive symptoms are clues to anatomic localization, attention to the details of responses in neuropsychological tests offers noninvasive, inexpensive opportunities for deeper study. Finally, novel experimental cognitive tests may be specifically applicable to lupus.
Table 2. Cognitive Tests for Patients with Lupus
National Adult Reading Test (NART) (to estimate IQ)*
Digit symbol substitution test
Trail-making test (part A and B)
Stroop color and word test
California verbal learning test
Rey Osterrieth complex figure test (with delayed recall)
Wechsler Adult Intelligence Scale (WAIS) III letter numbering sequencing*
Controlled oral word association test
Animal naming
Finger tapping

