A second observation was long-term persistence of FMc and MMc. A third observation was the predilection of autoimmune diseases in women, as well as the peak incidence of most autoimmune disease in post-reproductive years.
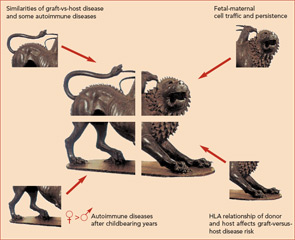
Finally, the observation that HLA relationships between a recipient and donor are critical determinants of graft-versus-host disease led to the proposal that excess HLA sharing (without complete HLA identity) might result in aberrant monitoring or interactions with microchimeric cell populations.
Microchimerism in SSc
The first report investigating microchimerism in an autoimmune disease was a prospective blinded study of FMc in women with SSc.11 FMc was measured by a quantitative test for male DNA in the peripheral blood of women who had sons. Significantly higher FMc levels were found in women with SSc compared with healthy women. Subsequent studies identified FMc in tissues of SSc patients.8 MMc has also been investigated in SSc. Unlike FMc the quantitative levels of MMc in SSc patients did not differ significantly from controls, although the prevalence (any positive result) was greater in SSc patients than controls.12 A theme that emerged from the beginning of studies of microchimerism was the importance of quantitative techniques—especially because both FMc and MMc are often found in healthy individuals without autoimmune disease but usually at low levels.
As the goal for microchimerism studies of SSc is to generate new therapeutic approaches for this difficult disease, the next question to address is how might naturally acquired microchimerism contribute to SSc? Considering an analogy with graft-versus-host disease where donor T lymphocytes are thought to mediate disease, if fetal T cells were implicated in disease pathogenesis, these cells could be selectively targeted. However, this explanation is unlikely both because of radical differences in the extent of chimerism in the two disorders and because FMc is found among T cells in healthy individuals as well as SSc patients. Indeed both FMc and MMc are found in T and B cells, monocyte/macrophages, and NK cells.13
A more likely analogy with SSc is the situation that occurs in chronic organ graft rejection. In this setting, recipient cells react with other recipient cells but aberrant immunity occurs because fragments of HLA molecules from the chimeric donor cells are being presented for immune recognition. In this case, a future therapeutic approach could be HLA peptide inhibitors that block the interaction between antigen presenting cell and T lymphocyte or compete with foreign peptides to induce tolerance rather than stimulate the T cell. Another area of active investigation in autoimmunity is the role of T regulatory cells. Important in limiting autoreactive T cells, T regulatory cells are increased in the mother during pregnancy and in cord blood and may be important in tolerance to FMc after pregnancy. If aberrant T regulatory function is found, a deficit could potentially be restored by adoptive cellular therapy.
Microchimerism in Juvenile Myositis
In studies of patients with juvenile dermatomyositis and idiopathic myositis, MMc was found in muscle biopsies but was infrequent in muscle biopsies from other diseases.14,15 Studies were performed by selecting male patients and identifying female cells in the biopsy samples. The study of dermatomyositis also found that patients had MMc in peripheral blood significantly more often than their unaffected siblings.14 Peripheral blood studies were performed by DNA testing for maternal-specific, non-shared HLA. In further studies, chimeric maternal T lymphocytes isolated from dermatomyositis patients reacted to the patient’s cells, producing interferon-g in vitro, but chimeric maternal cells from unaffected siblings did not react to the sibling’s cells.16 Thus, the investigators proposed that chimeric maternal T lymphocytes are effectors of disease in myositis patients.

