Studies on the relationship between inflammation and syndesmophyte formation in AS patients suggest that these bony bridges tend to form at sites of vertebral inflammation, but most often after the inflammation has resolved.23–25 If these data are confirmed, they would suggest that although TNF-a–driven inflammation could be an important prerequisite to abnormal bone formation, the two processes may be mediated by different factors. If this is the case, TNF-a blockade very early in the course of disease might be beneficial, while later in disease it might permit new bone formation to proceed. There may be additional targets to inhibit pathological bone formation.
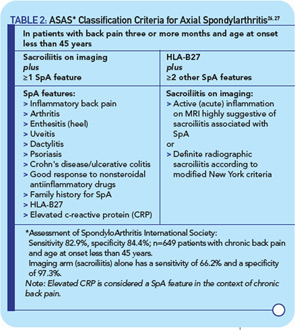
Identifying patients very early in the course of disease before the development of radiographic changes (and hence before they meet criteria for AS) has become a high priority in SpA research. The Assessment of SpondyloArthritis International Society (ASAS) workgroup recently reported criteria that identify patients with preradiographic axial SpA.26,27 This important advance was accomplished through a consensus approach using expert opinions and then validated in a multicenter study. The new criteria identify individuals with preradiographic axial SpA as well as those that meet the stricter modified New York criteria for AS and thus capture a large spectrum of axial disease (see Table 2, at right).
The new classification criteria incorporate evidence of active sacroiliitis on MRI or plain films, together with other clinical or laboratory features of SpA, most of which were included in the European Spondyarthropathy Study Group or Amor criteria that defined undifferentiated SpA. The axial SpA category includes individuals with psoriasis, dactylitis, and/or IBD. In 649 patients with chronic back pain who were younger than age 45 years, sensitivity and specificity were 83% and 84%, respectively. The ASAS group also refined clinical criteria for inflammatory back pain, which is now considered as chronic back pain (greater than or equal to three months in duration) of insidious onset, beginning at 40 years of age or younger, that improves with exercise but not with rest, and occurs at night with improvement on getting up. The new axial SpA criteria will enable clinical trials to address whether early aggressive treatment changes the course and outcome of disease, in particular the development and progression of bony changes such as osteophytes and syndesmophytes.
Treatment of SpA in Children
Current approaches to the treatment of SpA in children are based largely on clinical experience, because no controlled clinical trials have been published. Guidelines for adult patients with AS established by ASAS and modified by SPARTAN (an organization that fosters SpA research and education) for the U.S. population would be applicable to only the fraction of children who meet modified New York criteria.28 In patients with disease more broadly defined as pediatric SpA (such as ERA), nonsteroidal antiinflammatory drugs can help reduce inflammation and pain but are rarely adequate to control disease; there is no evidence that sulfasalazine or methotrexate are beneficial.29 Activity and physical therapy are widely recommended and considered to be beneficial, but more evidence is needed to better define the role of these modalities.