In addition to small vessel vasculitis and infective endocarditis, ANCA testing can also be positive in inflammatory bowel disease, rheumatoid arthritis, systemic lupus erythematosus, human immunodeficiency virus (HIV) infection, malignancies and as a reaction to certain pharmaceuticals.6 Therefore, it can be incredibly difficult to distinguish between an infective endocarditis with a positive ANCA and an ANCA-associated vasculitis with endocardial involvement.
We describe the case of an elderly woman who presented with historical, physical, laboratory and echocardiographic findings consistent with infective endocarditis, including a vegetation on the mitral valve, who was ultimately determined to have GPA and managed with immunosuppressive therapy.
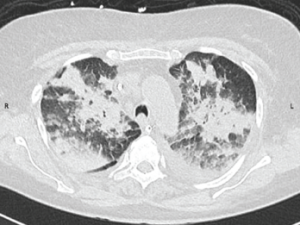
Figure 1: CT Scan of the Chest
A CT scan of the chest obtained without intravenous contrast demonstrates diffuse patchy and groundglass opacifications with upper lobe predominance. These findings are consistent with pulmonary hemorrhage. In addition, bilateral pleural effusions are seen.
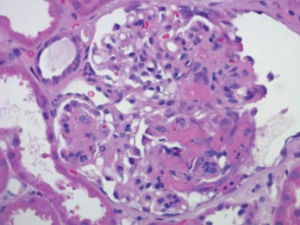
Figure 2: Renal Biopsy
Biopsy specimen of the kidney stained with hematoxylin and eosin demonstrates a necrotizing glomerulonephritis with a fibrinous crescent within the glomerulus. Immune-complex deposits were not seen on electron microscopy (image not shown).
Case Report
A 78-year-old Caucasian woman presented to an outside hospital with a one-week history of shortness of breath and diffuse joint pains in her bilateral knees and shoulders. Her medical history included hypertension not controlled by any medications, an appendectomy, multiple family members with rheumatoid arthritis and a five pack-year smoking history. She did not take any medications at home. Three weeks prior to presentation, she underwent a tooth extraction for a dental abscess and was given a course of penicillin.
On presentation, she was afebrile with a blood pressure of 195/85 mmHg and a heart rate of 150 beats per minute. Further examination demonstrated a III/VI systolic murmur heard across the precordium. A petechial rash was present on the right lower extremity, and splinter hemorrhages and Osler nodes were present on the fingers of both hands. Her laboratory studies were notable for a total leukocyte count of 13,000 cells/μL, and her electrocardiogram (ECG) demonstrated first-degree atrioventricular block. Her urine culture grew Escherichia coli, for which she was started on ceftriaxone.
Blood cultures drawn three days after initiation of ceftriaxone treatment were negative. She subsequently developed a cough productive of mucopurulent sputum that progressed to hemoptysis and hypoxemic respiratory failure, and required endotracheal intubation. A computed tomography (CT) angiogram of the chest ruled out pulmonary embolism, but demonstrated focal consolidations consistent with multifocal pneumonia. A bronchoscopy revealed bleeding from the left upper lobe without any lesions. Transesophageal echocardiogram (TEE) demonstrated mitral and aortic valve thickening with a small vegetation on the mitral valve. Infective endocarditis was suspected, and the patient’s antibiotic therapy was broadened to ceftriaxone and vancomycin.

