Back pain is a frequent complaint in rheumatology practices. Many patients, and older patients in particular, who present with back pain have the clinical syndrome of lumbar spinal stenosis (LSS). This article discusses several of the most daunting challenges of diagnosis and treatment of LSS, and suggests possible approaches.
Diagnostic Challenges
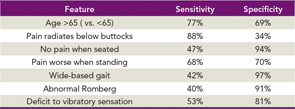
- The characteristic history and physical examination findings of spinal stenosis are nonspecific and insensitive. The characteristic history elicited from patients with symptomatic LSS features neurogenic claudication, a syndrome characterized by two key components. The first is radiation of the pain beyond the lumbar region. The pain of spinal stenosis typically originates in the back and radiates into the buttocks and sometimes into the thighs, lower legs, and feet. Unlike sciatica due to a herniated disk, which typically radiates in a discrete dermatomal pattern into the calves and feet, the pain of spinal stenosis often radiates more diffusely into the buttocks and upper thighs and no further. The second notable feature of neurogenic claudication is a postural component. Patients feel less pain when they are flexed forward at the spine, as in sitting, and more pain when they are extended, as in standing and walking. As Table 1 shows, the pain location and the provocation with extension and relief with flexion are diagnostically useful, but neither is perfectly sensitive nor specific.
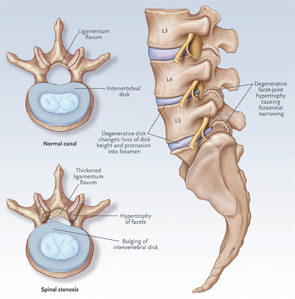
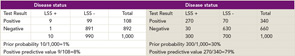
- Imaging tests are super-sensitive and nonspecific. The key imaging features of degenerative lumbar spinal stenosis are shown in Figure 1. These include facet joint hypertrophy and ligamentum flavum hypertrophy and disc protrusion. The combination of these findings can result in central or neuroforaminal stenosis. The problem is that the imaging features of lumbar spinal stenosis are very common in asymptomatic individuals. Stenosis is observed on magnetic resonance imaging (MRI) in more than 20% of asymptomatic patients older than age 60.The diagnostic utility of an MRI positive for LSS varies according to the prior probability, which refers to the clinician’s estimate of the probability of disease before the test was performed. When the prior probability is low, say just 1%, a positive test will often turn out to be a false positive, even if the test has high sensitivity and specificity. Table 2 provides examples of prior probabilities and corresponding posttest probabilities (or positive predictive values) for a test with sensitivity and specificity of 90%. In this two-by-two table analysis, the prevalence of LSS represents the pretest probability. This table makes the point that same test has very different positive predictive values in situations of low prior probability versus higher prior probability. In the situation on the left side of the table, the prior probability, as represented by the prevalence of disease, is 1% and the posttest probability, or positive predictive value, is 8%. On the shaded right half of the table, with a prior probability of 30%, the posttest probability or positive predictive value is 79%. Thus, in the first scenario, the vast majority of positive tests are false positives. In the second scenario, four of five positive tests are true positives.
- The diagnosis of spinal stenosis frequently coexists with other common problems. These problems include osteoarthritis of the hips, trochanteric bursitis, facet syndrome, vertebral fracture, nonspecific low back pain, and vascular claudication. Clinicians must distinguish among this array of possible diagnoses to identify the primary source of pain for any particular patient. These other disorders are not necessarily difficult to identify (trochanteric bursitis and hip osteoarthritis, for example, are relatively easy diagnoses to establish); the challenge is determining which of several coexisting problems is responsible for most of the patient’s symptoms.
Potential Solutions to These Diagnostic Challenges
It is important for clinicians to listen and examine carefully, and to form an impression based on the history of physical examination findings, the patient’s age, and other such clues. If the clinician senses that spinal stenosis is reasonably likely on the basis of several history and physical examination findings, imaging tests can be useful in confirming the diagnosis. On the other hand, when the clinical picture is not compelling, imaging tests are much less valuable because positive tests are frequently misleading. If imaging tests are performed under similar circumstances, a positive imaging test (or a single positive element of the history or physical examination, for that matter) can often be disregarded.
The problem of coexisting diagnoses requires some creativity on the part of the clinician. It is often helpful to use soft tissue and joint injections to isolate the source of symptoms. For example, trochanteric or hip injections (often done under fluoroscopy) are useful in ruling out the greater trochanter or hip as the primary source of symptoms. It is important not to mistake spinal stenosis for vascular claudication, and it is occasionally necessary to obtain ankle brachial index evaluations to identify vascular compromise. Generally, however, these entities can be distinguished by history, as the postural element of lumbar stenosis (such as exacerbation with lumbar extension) is typically not observed in patients with vascular claudication.

It is useful to work carefully with a surgeon who is thoughtful, conservative, and able to simplify the complicated details and concepts of spinal arthrodesis when explaining the options to patients…There is no evidence that surgery needs to be performed promptly in patients with spinal stenosis. Thus, patients can—and should—take their time in making these decisions.
Challenges in Treating Spinal Stenosis
- Exercise is frequently prescribed for lumbar spine problems, but is difficult for patients with spinal stenosis. It can be very challenging for patients with stenosis to run or walk even short distances, or to stay standing for any period of time. The problem is that lumbar extension exacerbates compression and therefore exacerbates symptoms.
- Medications used to treat pain are not tolerated well in the elderly, who comprise the majority of spinal stenosis patients. Nonsteroidal antiinflammatory drugs (NSAIDs) are often useful in reducing pain in patients with spinal stenosis and other spine problems. However, patients over the age of 60 often have gastrointestinal intolerance, and many take anticoagulants or have risk factors for cardiac disease. Because nonselective NSAIDs increase bleeding risk and both nonelective and particularly selective NSAIDs pose a risk of cardiac events, these problems complicate the choice of medications. Celecoxib can overcome the problem of bleeding risk but poses an additional risk of cardiac disease, which is frequently concerning to patients and their physicians. Narcotic medications are another option, but they are also often tolerated poorly in the elderly, who are at risk of falls and other adverse events. Acetaminophen is generally tolerated well, though it frequently provides inadequate pain relief and the dose must be watched carefully to avoid the risk of liver disease.
- Older patients are often risk averse and less willing to entertain invasive procedures than their younger counterparts. Lumbar epidural steroid injections are short lived and lack high-quality trials demonstrating their efficacy. The observational literature suggests these injections have a role in relieving leg pain, though their effectiveness in relieving back pain is less clear. The principal risks associated with these procedures—infection and nerve damage—are less than 1%. Many patients have developed a fear of spinal injections from friends and family who themselves have undergone similar injections and found them painful or experienced complications.
Lumbar laminectomy is effective in the management of lumbar stenosis. As with injections, surgery is especially helpful if the patient has a predominance of leg pain. A particularly challenging feature of the discussion of surgery for spinal stenosis is the role of lumbar arthrodesis, or fusion, which has a higher risk of complications than simple decompression. The indications for lumbar fusion are not well defined and require further study, though the literature suggests that fusion benefits patients undergoing decompression who have a concomitant spondylolisthesis or scoliosis. There are several approaches to lumbar fusion, including autogenous arthrodesis (often using bone from the patient’s iliac crest) and supplementation of the autogenous bony fusion with instrumentation (e.g., pedicle screws, plates, fusion cages, and artificial discs). However, the literature on these types of implants is inadequate and controversial.
Strategies for Overcoming Treatment Challenges
Devising a treatment plan for spinal stenosis can be challenging. It is helpful to discuss these options with patients over the course of many visits. A potential solution to the problem of difficulty walking is for patients to do aerobic exercises that can be accomplished in flexion; stationary bicycling is a good example. The problem of medication intolerance is not easy to overcome. Patients with spinal stenosis often do well with acetaminophen as their principal medication along with low and intermittent doses of NSAIDs and low doses of opiates, particularly at night. Topical nonsteroidal medicine can be helpful as well. Some patients find acupuncture helpful, although there is no clear evidence to support the efficacy of acupuncture for pain relief in spinal stenosis. Patients with concomitant spondylolisthesis or scoliosis often have an instability component to their pain and benefit from periodic use of a lumbar corset. It is particularly important for specialists and the primary care physician to communicate clearly about medication use in older patients, as the risks of drug toxicity and interactions are high.
It is useful to work carefully with a surgeon who is thoughtful, conservative, and able to simplify the complicated details and concepts of spinal arthrodesis when explaining the options to patients. Minor neurologic deficits are not urgent indications for surgery, and there is no evidence that surgery needs to be performed promptly in patients with spinal stenosis. Thus, patients can—and should—take their time in making these decisions. The decision should be made electively, be based on symptoms, and involve thoughtful discussions between patients and their surgeon, rheumatologist or primary care doctor, and family.
Summary
LSS is a common and disabling problem, and its prevalence will increase over the coming years with the aging of the population. The diagnosis can be challenging to make because the history, physical examination, and imaging findings are either insensitive, nonspecific, or both. Further, the clinician must distinguish between LSS and coexisting diagnoses, such as bursitis or osteoarthritis, to identify the primary cause of symptoms. After arriving at a diagnosis, clinicians must navigate the additional challenges of both the operative and nonoperative treatments for this condition. There is no “correct” decision regarding use of conservative therapy, injections, and surgery. Clinicians and patients should engage in a shared decision-making process and arrive at a decision that is consonant with the patient’s values.
Acknowledgment: I appreciate the editorial assistance and advice of Julian Prokopetz in preparing this manuscript.
Dr. Katz is professor of medicine and orthopedics with the department of orthopedics and the division of rheumatology, immunology, and allergy at Brigham and Women’s Hospital and Harvard Medical School, Boston, Mass.
Additional Reading

- Katz JN, Dalgas M, Stucki G, et al. Degenerative lumbar spinal stenosis: Diagnostic value of the history and physical examination. Arthritis Rheum. 1995;38:1236-1241.
- Katz JN, Harris MB. Clinical practice: Lumbar spinal stenosis. N Engl J Med. 2008;358:818-825.
- Suri P, Rainville J, Kalichman L, Katz JN. Does this older adult with lower extremity pain have the clinical syndrome of lumbar spinal stenosis? JAMA. 2010;304:2628-2636.
- Jensen MC, Brant-Zawadzki MN, Obuchowski N, Modic MT, Malkasian D, Ross JS. Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med. 1994;331:69-73.
- Deyo RA, Mirza SK, Martin BI, Kreuter W, Goodman DC, Jarvik JG. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA. 2010;303:1259-1265.
- Weinstein JN, Tosteson TD, Lurie JD, et al. Surgical versus nonsurgical therapy for lumbar spinal stenosis. N Engl J Med. 2008;358:794-810.