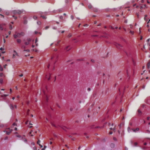
In a first randomized controlled trial-derived longitudinal study, researchers found that a disease-modifying anti-rheumatic drug (DMARD) and etanercept, a biologic DMARD (bDMARD), in treatment-naive, early rheumatoid arthritis (RA) patients free of known cardiovascular disease (CVD) reduced vascular function abnormalities measured by cardiac MRI. Findings from the Coronary Artery Disease Evaluation in Rheumatoid Arthritis (CADERA) study suggest this treatment strategy may influence aortic distensibility more than disease activity and that there may be a treatment advantage of etanercept+ methotrexate over methotrexate with or without additional conventional synthetic disease-modifying anti-rheumatic drugs (csDMARDs).1
In a first randomized controlled trial-derived longitudinal study, researchers found that a disease-modifying anti-rheumatic drug (DMARD) and etanercept, a biologic DMARD (bDMARD), in treatment-naive, early rheumatoid arthritis (RA) patients free of known cardiovascular disease (CVD) reduced vascular function abnormalities measured by cardiac MRI. Findings from the Coronary Artery Disease Evaluation in Rheumatoid Arthritis (CADERA) study suggest this treatment strategy may influence aortic distensibility more than disease activity and that there may be a treatment advantage of etanercept+ methotrexate over methotrexate with or without additional conventional synthetic disease-modifying anti-rheumatic drugs (csDMARDs).1
This study highlights the importance of identifying patients at risk of CVD early as a management strategy, according to Maya H. Buch, MD, PhD, co-investigator of the study and a rheumatologist at the Leeds Institute of Rheumatic and Musculoskeletal Medicine, U.K. Dr. Buch reported these initial findings at the 2018 ACR/ARHP Annual Meeting in Chicago. “These findings also confirm RA therapy, without specific CVD therapy, improves CVD changes, thus, implying atherosclerosis comprises inflammation that is amenable to RA therapy.”
Dr. Buch says, “If the suggestion of differential benefit between the two treatment strategies is proved in the future, this would expand the remit of personalized/stratified therapy, [indicating] we should be tailoring therapy [not just] to traditional outcomes of RA, but also [to] CVD.”
The CADERA Study
In this phase of the CADERA study, 80 patients with early RA (defined as symptomatic for less than 12 months) who had no prior RA therapy and no history of CVD were randomized into two groups. Group 1 received first-line etanercept, a TNF inhibitor (TNFi) bDMARD, plus methotrexate. Group 2 received methotrexate in a treat-to-target planned escalation to a triple, conventional synthetic (cs) DMARD (methotrexate, sulphasalasine, and hydroxychloroquine). At Week 24, patients in Group 2 who failed to achieve clinical remission were switched to etanercept plus methotrexate (referred to as escalated patients).
At Week 48, the etanercept was stopped in both groups and standard-of-care treatment comprising csDMARD with or without bDMARD as per the National Institute for Health and Care Excellence (NICE) and local guidance was maintained with observation up to Week 96. The changes in aortic distensibility value from baseline were then evaluated.
All patients, including patients from Group 2, demonstrated a significant reduction in mean aortic distensibility from baseline through Year 1, with these results maintained at Year 2.
Previously reported work from the CADERA study includes study protocol and demonstrated abnormalities in vascular and myocardial function of treatment-naive, early RA patients.2,3
Outlook for Practice
Dr. Buch and her co-investigators plan to validate this study through a larger trial to investigate if etanercept plus methotrexate has a greater benefit over standard initial methotrexate and/or additional csDMARD treatment. Additionally, they are conducting parallel experimental genomic, transcriptomic and proteomic work on bio-samples collected from study participants to further understand the mechanisms identified in these most recent findings.
Through this additional investigation, Dr. Buch suggests longer follow-up and time points could provide a high-resolution assessment of the relationship between the trajectories of disease activity and cardiac MRI abnormalities, and could introduce a study approach in which patients are stratified based on CVD risk.
If applied in practice at diagnosis, this approach would better inform treatment choice, including whether targeted therapy with a TNFi such as etanercept, may be indicated in some patients, Dr. Buch explains.
On sharing these findings at the Annual Meeting, Dr. Buch says the discussion centered on how the rheumatology community is at risk of dismissing the importance of CVD comorbidity by suggesting it has been fully addressed with improved diagnosis and more effective therapies. “Our ambition should be to refine practice, and with a more cost-effective biologic drug landscape, this could be more viable.”
Carina Stanton is a freelance science journalist based in Denver.
References
- Buch MH, Erhayiem B, Fent G, et al. Treatment-naïve, early rheumatoid arthritis patients demonstrate reversible abnormalities of vascular function on vardiac MRI with RA therapy with preliminary suggestion of greater improvement with anti-TNF compared to MTX/conventional therapy—a first, RCT derived longitudinal study [abstract]. Arthritis Rheumatol. 2018 Oct;70(suppl 10).
- Erhayiem B, Pavitt S, Baxter P, et al. Coronary Artery Disease Evaluation in Rheumatoid Arthritis (CADERA): Study protocol for a randomized controlled trial. Trials. 2014 Nov 8;15:436.
- Erhayiem B, McDiarmid A, Swoboda P, et al. Treatment-naïve, early rheumatoid arthritis patients demonstrate abnormalities of vascular and myocardial function on cardiac MRI [abstract]. Arthritis Rheumatol. 2015 Oct; 67 (suppl 10).