In SSc, the incidence of sudden cardiac death is higher than that in the general population. Postmortem studies of SSc patients who die suddenly show a history of ventricular arrhythmias, documented ventricular tachycardias, and frequent multifocal premature ventricular contractions.4 Currently, there is no evidence that drug therapy lowers mortality in SSc patients. In fact, the outcome may be even worse with treatment because of a proarrythmic effect of drugs; the use of drugs, however, may represent a marker of severity of arrhythmia rather than a cause of increased mortality. Whatever the basis for this association, these data suggest that use of anti-arrhythmics in SSc patients should be closely monitored with repeated ambulatory electrocardiography.
Diagnosis
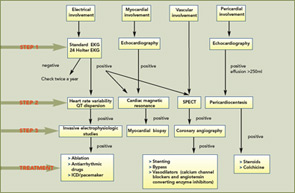
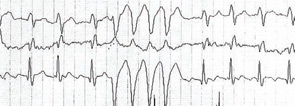
1) Standard 12-lead electrocardiogram (EKG): At baseline, a standard 12-lead EKG with serial studies at intervals is the most simple, inexpensive, and rapid method for initial cardiac evaluation (see Figure 1, p.17). In SSc, an EKG can detect hidden arrhythmias, asymptomatic conduction defects, and previous ischemic defects. In a large EKG study, ventricular ectopy occurred in 67% of patients and was strongly correlated with total mortality and sudden death, independently from other indexes of severity of disease and organ involvement.
2) Holter monitoring: Holter monitoring is a non-invasive method with high predictive value that permits the early detection of cardiac involvement. Analysis of Holter monitoring data can detect arrhythmias and conduction defects not seen on a standard EKG. Patients with significant abnormalities on Holter monitoring should have further investigations (see Figure 1, p.17). In SSc, Holter monitoring may add valuable information about the autonomic nervous system, assessing the heart rate variability and the QT interval. Recently, abnormalities of heart rate variability and increased QT dispersion have been reported in SSc patients. Autonomic dysfunction represents the cardiac vulnerability resulting from an autonomic imbalance and is a marker for arrhythmic death or an indicator of disease severity. We strongly recommend performance of a Holter at least twice a year in patients with SSc.
3) Invasive electrophysiologic studies: Invasive electrophysiologic studies are indicated when spontaneous arrhythmias are frequent and when a serious sustained arrhythmia is suspected. Electrophysiologic studies can detect the mechanism generating the arrhythmias and allow the selection of patients who can be treated by transcatheter ablation; in this selection, the guidelines are similar to those employed in the management for ventricular tachycardia due to coronary disease.5
Treatment
At present, the management of cardiac involvement in SSc remains largely empirical and derives mainly from evidence obtained from other diseases. There is no evidence that anti-arrhytmic drug therapy lowers mortality in SSc patients. Successful treatment with ablation, both surgical cryoablation and catheter ablation, has been reported. Implantation of a cardioverter defibrillator and/or a pacemaker may be a treatment of choice for patients with life-threatening ventricular arrhythmias and conduction defects.
Myocardial Piece of the Puzzle
Primary myocardial involvement in SSc is characterized by patchy fibrotic lesions distributed in both ventricles. Although advanced myocardial fibrosis may lead to congestive heart failure, systolic or diastolic dysfunction can occur early in the disease, before becoming symptomatic years later. When clinically evident, myocardial involvement is recognized as a poor prognostic factor since the overall mortality rate at five years of SSc patients with proven cardiovascular impairment is over 70%. Usually, physical findings are nonspecific and include signs of congestive heart failure. For this reason, a timely diagnosis is highly recommended.
