ACR CONVERGENCE 2021—In a session on the diagnosis and treatment of interstitial lung disease (ILD) in patients with rheumatic diseases, Melissa Griffith, MD, assistant professor of medicine at the University of Colorado Anschutz Medical Campus, Aurora, Colo., began her presentation by reviewing common presentations of autoimmune lung disease.
ACR CONVERGENCE 2021—In a session on the diagnosis and treatment of interstitial lung disease (ILD) in patients with rheumatic diseases, Melissa Griffith, MD, assistant professor of medicine at the University of Colorado Anschutz Medical Campus, Aurora, Colo., began her presentation by reviewing common presentations of autoimmune lung disease.
“These are exceedingly rare diseases, with a paucity of trials and data,” said Dr. Griffith.
CTD-Associated ILD
“Patients with [ILD] may not yet have [an] identifiable rheumatic disease, but many eventually develop one,” said Dr. Griffith.
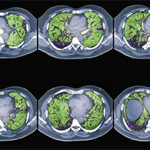
The most common patterns of ILD in connective tissue disease (CTD) are interstitial pneumonia, nonspecific interstitial pneumonia, organizing pneumonia and lymphocytic interstitial pneumonia.1 According to Dr. Griffith, these patterns are important because they guide prognosis. She emphasized that high-resolution computed tomography (CT) is crucial for diagnosing pulmonary fibrosis and should be used instead of traditional CT or chest radiographs.2
Diagnosis will likely require input from multiple healthcare providers. Dr. Griffith reinforced this point with data from a multidisciplinary ILD clinic at Massachusetts General Hospital, Boston. Researchers evaluated 50 patients referred to the tertiary care practice over a 12-month period. Patients were independently assessed by a rheumatologist and a pulmonologist. The investigators found the diagnosis was changed in 54% of patients who presented to the ILD clinic. Moreover, the evaluation resulted in changes in therapy for 80% of patients with CTD-associated ILD and 27% of patients with idiopathic pulmonary fibrosis. The authors concluded that rheumatologists should play a significant role in the clinical care of these patients and evaluate all patients with ILD.3
Rheumatologists should obtain autoimmune serologies on most patients with ILD, said Dr. Griffith, because this information can be useful in guiding therapy. Example: In the PANTHER-IPF trial, patients with idiopathic pulmonary fibrosis treated with a combination of prednisone, azathioprine and N-acetylcysteine were found to have higher risks of hospitalization and death than patients treated with placebo.4
“This [finding] led to a fundamental change in the way pulmonologists treat idiopathic pulmonary fibrosis,” explained Dr. Griffith.
Scleroderma-Associated ILD
In this section of her presentation, Dr. Griffith explained that ILD does not affect all patients with scleroderma equally. Although approximately half of patients with scleroderma will eventually be diagnosed with ILD, the risk for ILD varies by the type of scleroderma. For patients with scleroderma who are diagnosed with ILD, poor prognostic features include disease duration of less than four years, diffuse scleroderma, forced vital capacity (FVC) of <65%, diffusing capacity of carbon monoxide (DLCO) of <55%, a finding of more than 20% lung involvement as determined by high-resolution CT and SCL-70 antibody positivity.
Dr. Griffith treats patients with scleroderma-related ILD with mycophenolate mofetil, tocilizumab and cyclophosphamide. Other treatment options include azathioprine and rituximab. She said nintedanib, an antifibrotic medication, was recently approved for the treatment of chronic, fibrosing ILD, with a progressive phenotype, and another antifibrotic, pirfenidone, is currently in clinical trials.
Dr. Griffith also emphasized that it’s important to treat gastroesophageal reflux disease in this patient population. She recommended proton pump inhibitors and histamine H2-blockers, as well as elevating the head of the bed and modifying a patient’s diet to avoid trigger foods and avoid late meals. Some patients, she said, may also benefit from esophagogastroduodenoscopy with esophageal dilation.
Approximately half of patients with scleroderma will eventually be diagnosed with ILD, but the risk for ILD varies by the type of scleroderma.
RA-Associated ILD
Dr. Griffith asks her patients with rheumatoid arthritis (RA) about respiratory symptoms at every visit. She also carefully examines patients with RA for pulmonary rales. If patients have symptoms or pulmonary function test progression, she orders a high-resolution CT scan. For patients with significant lung disease, she performs pulmonary function tests every three to six months.
MDA5 Dermatomyositis & ILD
“MDA5 is a bad actor for [ILD],” said Dr. Griffith, adding, “These patients are at high risk from dying from their lung disease.”
She emphasized that young patients with rapidly progressive ILD and rashes should be evaluated for myositis, with the recognition that their autoantibody profile can be important for prognosis.
Dr. Griffith often treats these patients with glucocorticoids and cyclosporine A or tacrolimus. “This is a really heavy regimen, but it is sometimes necessary, considering how sick these patients get,” she said.
Interstitial Pneumonia with Autoimmune Features
Patients with interstitial pneumonia have some features of autoimmunity, but do not have a characterizable CTD. Dr. Griffith looks for key features of autoimmunity in these patients and considers a biopsy if these features are unclear. She relies heavily on the expertise of pathologists and radiologists, and if she feels a patient has the features of interstitial pneumonia with autoimmunity, she prescribes immunosuppression.
Lara C. Pullen, PhD, is a medical writer based in the Chicago area.
References
- Fischer A, du Bois R. Interstitial lung disease in connective tissue disorders. Lancet. 2012 Aug 18;380(9842):689–698.
- Mueller-Mang C, Grosse C, Schmid K, et al. What every radiologist should know about idiopathic interstitial pneumonias. Radiographics. 2007 May–Jun;27(3):595–615.
- Castelino FV, Goldberg H, Dellaripa PF. The impact of rheumatological evaluation in the management of patients with interstitial lung disease. Rheumatology (Oxford). 2011 Mar;50(3):489–493.
- Idiopathic Pulmonary Fibrosis Clinical Research Network. Prednisone, azathioprine, and N-acetylcysteine for pulmonary fibrosis. N Engl J Med. 2012 May 24;366(21):1968–1977.