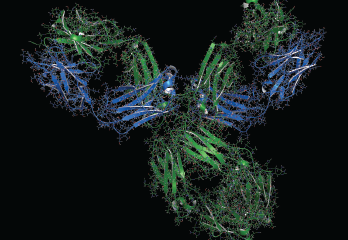
A 3-D rendering of pembrolizumab monoclonal
antibody drug protein, an immune checkpoint inhibitor targeting PD-1.
molekuul_be / shutterstock.com
CHICAGO—The body of literature on immunosuppressive drugs used to treat cancer and autoimmune diseases is growing, helping bring some clarity to their effects on the immune system and how well they work in patients. This has helped refine the questions that further research must answer, said an expert at the 2018 ACR/ARHP Annual Meeting.
The need for reliable information to guide clinicians is obvious: A “tidal wave of cancer immunotherapy” is hitting, with the approach now considered the fourth pillar of cancer treatment alongside the mainstays of surgical removal, chemotherapy and radiation, said Leonard Calabrese, DO, head of the Clinical Immunology Division at Cleveland Clinic, Ohio.
When activated, immune checkpoints, such as CTLA4 and PD-1 (the two prominent players in cancer treatment thus far), downregulate activated T cells, tamping down the immune response. Inhibiting them enhances the immune response. More than 160 checkpoint inhibitors (CPIs) are in preclinical and clinical trials, so their presence on the cancer stage will grow more pronounced, Dr. Calabrese said.
These two categories of CPIs, research suggests, impose their effects in different ways that could have important clinical meaning, he said. A recent review described the effect of CTLA-4 inhibition (as well as chimeric antigen receptor [CAR] T cells) as “immuno-enhancement,” and that of PD-1 and PD-L1 inhibitors as “immuno-normalization.”1
The authors describe immunity as water flowing through a pipe and cancer as a plug in the pipe once it “gets the upper hand,” Dr. Calabrese said. CTLA-4 inhibition relies more on increasing the water pressure to push out the plug—that is, revving up the immune system to fight the tumor—whereas PD-1 and PD-L1 inhibition is more like simply removing the plug, or steering the immune response more directly at the tumor.
“Until recently, all immunotherapy was considered immune enhancement; in other words, pushing the immune system through,” Dr. Calabrese said. “The introduction, particularly of PD targeting, … should be reconceptualized as to actually immune-normalize … because most of the activity is going on within the tumor microenvironment.”
Researchers are busy trying to tackle the question of how closely checkpoints and autoimmunity are linked. “The real action right now is in … trying to frame important questions to answer whether there is evidence checkpoints’ dysfunction is operative in the pathogenesis of autoimmune disease, and, in particular, rheumatic autoimmune disease,” he said.