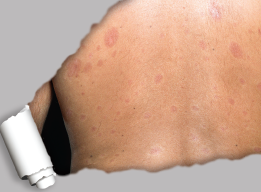
Skin plaques in systemic sclerosis.
SPL / Science Source
What happens when systemic sclerosis (SSc) overlaps with other systemic autoimmune rheumatic diseases? Patients with either diffuse cutaneous or limited cutaneous SSc sometimes develop systemic lupus erythematosus (SLE) as well. A new, large cohort study published in the Journal of Rheumatology reveals details on the epidemiology, clinical signs and survival data of SSc-SLE overlap syndrome.1
“Little is known on this group of patients, and it is important to shed light on their prevalence and characteristics,” says Sindhu R. Johnson, MD, PhD, director of the Toronto Scleroderma Project at the University of Toronto, Canada, and a study co-author. “The field of overlap syndromes has been challenging for clinicians. There is a lack of understanding and knowledge about what overlap means in terms of potential complications and prognosis. We do not have clearly specified diagnostic criteria or classification criteria to systemically identify these people.”
Past evidence shows SSc-SLE overlap patients more frequently present with Raynaud’s phenomenon and such complications as discoid lupus, lupus nephritis, pancreatitis, avascular bone necrosis and shrinking lung syndrome.2-6 Evidence also shows anti-U1RNP antibodies are more frequent in SSc-SLE overlap syndrome, and this study revealed more important serological markers.7 Anti-RNP or anti-U1RNP may be useful screening tests for SSc overlap syndromes, says Dr. Johnson.
Young, Female, Asian
The study’s cohort included subjects from the Toronto Scleroderma Program (a network of three academic hospitals) who fulfilled the ACR/European League Against Rheumatism (EULAR) classification criteria for SSc and/or the ACR classification criteria for SLE.8-10 The primary outcome was time from diagnosis to all-cause mortality. Patients were followed every 6–12 months using a standardized protocol. The study period ran from 1970–2017.
Out of 1,252 subjects, the researchers identified 1,116 with SSc only and 86 with SSc-SLE overlap syndrome, a prevalence of 6.8%. The overlap syndrome subjects were 92% female and 10 years younger at diagnosis than SSc patients who did not have SLE (a mean age of 37.9 vs. 47.9 years). In addition, compared with SSc patients without SLE, overlap syndrome patients in the study were more commonly of East Asian or South Asian ancestry.
Compared with SSc patients without SLE, overlap syndrome patients more frequently had lupus anticoagulant, anti-cardiolipin antibodies and pulmonary arterial hypertension (PAH). Less frequently, overlap patients had calcinosis, telangiectasia and diffuse subtype. The study found no significant differences between the two groups when it came to the occurrence of renal crisis, interstitial lung disease (ILD) or digital ulcers.
Patients in the two groups had no significantly different occurrences of comorbidities like hypertension, diabetes, dyslipidemia, cancer, stroke or atrial fibrillation. All of the SSc-SLE overlap syndrome patients had anti-dsDNA or anti-Sm antibodies.
No survival data had been reported for SSc-SLE overlap syndrome before this study. There were 432 deaths recorded during the follow-up, including 411 subjects with SSc alone and 21 with SSc-SLE overlap. Overlap syndrome patients had a better, but not statistically significant, difference in mean survival time: 26.1 years compared with 22.4 years for patients with SSc alone. Overlapping SLE neither increases the risk of, nor offers any protective effect against, mortality, the study found.

