Two helpful resources Dr. Weiss identified were the 2019 ACR/Arthritis Foundation guideline for the treatment of JIA and the updated recommendations for the treatment of ankylosing spondylitis and nonradiographic axial spondyloarthritis published jointly by the ACR, the Spondylitis Association of America and the Spondyloarthritis Research and Treatment Network.4,5
TMJ in JIA
In the session’s next talk, Randy Cron, MD, PhD, professor of pediatrics and medicine at the University of Alabama at Birmingham and director of the division of pediatric rheumatology at Children’s of Alabama, Birmingham, discussed temporomandibular joint (TMJ) involvement in JIA. Dr. Cron noted that about 40–80% of children with JIA will develop TMJ arthritis over the course of their disease and that all subtypes of JIA can involve this joint.
TMJ arthritis is frequently asymptomatic at the time of presentation. Thus, a detailed physical examination is needed to demonstrate decreased ability to open the jaw. MRI may also be a helpful diagnostic test to evaluate for the condition. Dr. Cron said one reason to care about this issue—aside from alleviating pain and symptoms—is that inflammation of the TMJ can lead to growth plate arrest and subsequent micrognathia. To spare children a poor outcome, early diagnosis is key. This approach is particularly challenging because TMJ arthritis can be active while other joints are in remission and because TMJ arthritis can develop even while patients are being treated with systemic therapies, including tumor necrosis factor-α inhibitors.
Treatment: Dr. Cron noted that an intra-articular corticosteroid injection can be effective in the short term to treat TMJ arthritis and is likely safe in adolescents. However, repeated intra-articular corticosteroid injections may be a risk factor for heterotopic bone formation in the joint.
In a retrospective study of 238 children with JIA who had received at least one intra-articular corticosteroid injection into the TMJ, 14% of patients developed heterotopic bone formation, with no cases diagnosed prior to the initial corticosteroid injection. The authors of the study explained that prospective studies are needed to delineate the risks posed by the injections as opposed to the risks associated with underlying disease activity. Clearly, the initiation of corticosteroid injections must be carefully considered.6
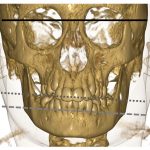
Imaging
In the final lecture, Ed Oberle, MD, RhMSUS, assistant professor of clinical pediatrics, the Ohio State University College of Medicine, Columbus, discussed the pros and cons of imaging in the management of JIA. At time of JIA diagnosis, imaging can be helpful to evaluate for and exclude other diagnoses. Example: Radiographs can reveal evidence of trauma, malignancy and congenital skeletal issues, and MRI can show evidence of pigmented villonodular synovitis, osteomyelitis and lipoma arborescens, among other conditions.