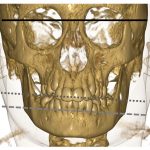
As noted in Dr. Cron’s presentation, imaging may be the only accurate way to detect early TMJ arthritis, and it’s important when evaluating for axial skeletal involvement. Dr. Oberle pointed out that common pitfalls in MRI include misinterpreting physiologic variability, such as bone marrow signal changes in healthy children that can resemble marrow edema, and that delay in contrast administration for contrast-enhanced images can result in over-enhancement and false positives.
Dr. Oberle discussed what the future may hold with regard to imaging for monitoring and assessment of treatment efficacy. Results of imaging modalities, such as ultrasound, can provide helpful information, such as surveillance for presence or absence of effusions, evaluation for joint or tendon enlargement, and assessment for active blood flow within tissue (i.e., a positive Doppler signal indicative of active synovitis).
However, identification of synovial hypertrophy alone does not necessarily mean there is active disease. Synovial hypertrophy may indicate either the start of a flare or represent remnant inflammation from a flare that has resolved. It’s true that imaging can be helpful to monitor for long-term damage, such as erosions, osteophytes, tendon thinning, tears and calcifications. A take-home message from Dr. Oberle’s talk was that imaging should represent one of many data points physicians use to diagnose and treat JIA.
The session as a whole was wide-ranging. By using an evidence-based approach to discuss these issues, the three speakers gave the audience an invaluable gift: insights from bench to bedside that can help refine clinical practice in the care of JIA.
Jason Liebowitz, MD, completed his fellowship in rheumatology at Johns Hopkins University, Baltimore, where he also earned his medical degree. He is currently in practice with Skylands Medical Group, N.J.
References
- Navid F, Holt V, Colbert RA. The enigmatic role of HLA-B*27 in spondyloarthritis pathogenesis. Semin Immunopathol. 2021 Apr;43(2):235–243. Epub 2021 Jan 22.
- Bridgewood C, Sharif K, Sherlock J, et al. Interleukin 23 pathway at the enthesis: The emerging story of enthesitis in spondyloarthropathy. Immunol Rev. 2020 Mar;294(1):27–47. Epub 2020 Jan 19.
- Weiss PF, Xiao R, Brandon TG, et al. Radiographs in screening for sacroiliitis in children: What is the value? Arthritis Res Ther. 2018 Jul 11;20(1):141.
- Ringold S, Angeles-Han ST, Beukelman T, et al. 2019 American College of Rheumatology/Arthritis Foundation guideline for the treatment of juvenile idiopathic arthritis: Therapeutic approaches for non-systemic polyarthritis, sacroiliitis and enthesitis. Arthritis Rheumatol. 2019 Jun;71(6):846–863. Epub 2019 Apr 25.
- Ward MM, Deodhar A, Gensler LS, et al. 2019 Update of the American College of Rheumatology/Spondylitis Association of America/Spondyloarthritis Research and Treatment Network recommendations for the treatment of ankylosing spondylitis and nonradiographic axial spondyloarthritis. Arthritis Rheumatol. 2019 Oct;71(10):1599–1613. Epub 2019 Aug 22.
- Stoll ML, Amin D, Powell KK, et al. Risk factors for intraarticular heterotopic bone formation in the temporomandibular joint in juvenile idiopathic arthritis. J Rheumatol. 2018 Aug;45(9):1301–1307. Epub 2018 May 15.