Alone Together
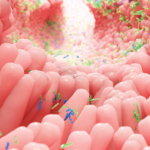
Not even the most solitary of all human beings is really ever alone. Indeed, we always have company, with the numerically greatest number of life companions small and invisible, and residing within inside us who, like Gulliver, are genuine giants in comparison. From the very moment we are born, an astounding, complex, and dynamic consortium of microorganisms occupies our body cavities (skin, airways, genitourinary, and gastrointestinal tracts) and coexists with us harmoniously as long as we breathe. This symbiotic relationship is based on a mutually beneficial exchange. We provide nutrients and an adequate environment for bacteria that, in return, shape our immune system, degrade complex polysaccharides, and produce vitamins and other essential factors we would otherwise be unable to produce.
The numbers are staggering. Consider these facts: The overall number of human cells in our bodies is about 10 trillion. The total bacterial cells we all carry at any given time nears 100 trillion. In fact, three pounds of bacteria reside in your intestines as you are reading! Therefore, on a cell-by-cell basis, we are only 10% human. And that isn’t all. A human genome contains roughly 30,000 protein-coding genes. The composite of microbial genome (or metagenome) is 100 times larger. By these metrics, we are 99% bacterial.
The complexity, power, and vastness of these “worlds within worlds” have led to the emerging field of microbiome, which has extended our view of self and transformed the common notion of individuality. Rather than unique and distinct individuals, according to emerging ideas, we should consider ourselves as ecosystems in which multiple species and their genes interact with each other in intricate ways to allow mutual survival.
I could not sufficiently wonder at the intrepidity of these diminutive mortals, who durst venture to mount and walk upon my body […] without trembling at the very sight of so prodigious a creature as I must appear to them.
—Jonathan Swift, describing Gulliver’s reaction to the Lilliputians, Gulliver’s Travels
The term “microbiome,” which was proposed a decade ago by Nobel laureate Joshua Lederberg, identifies the totality of microbes (commensals and pathogenic), their genomes (metagenome), and environmental interactions in a defined community or biological niche. Until recently, the microbial elements of biology have been all but ignored as determinants of health and disease beyond the obvious setting of infection.1
Most recently, and following the same logic, the National Institutes of Health Human Microbiome Project and the European MetaHit consortium have embraced the idea that it is impossible to fully understand human health and disease unless this collective human–microbiome “superorganism” is better studied and defined.2,3 This concept is attractive in understanding the pathogenesis of many rheumatic and autoimmune diseases and, more specifically, in rheumatoid arthritis (RA), which has long been regarded as a complex polygenic entity with an endless search for triggering factors.4
Dwarves Standing on the Shoulders of Giants
RA is a systemic, inflammatory autoimmune disorder. It is currently considered a multifactorial disease, in which multiple genes and environmental factors act in concert to cause pathological events.5 Despite recent advances in understanding molecular pathogenesis and developing more effective treatments, the etiology of RA remains mysterious, and treatment relies on agents that are broad in their action and fail to induce cure. Since the observation in the mid-1980s that the major histocompatibility complex class II alleles (“shared epitope” hypothesis) contribute to RA susceptibility, many other genetic variants associated with disease have been discovered through genome-wide association studies; these variants include PTPN22 and CTLA4, to name only two.4,6 Although genetic studies have improved our understanding of disease susceptibility and provided insight into functional genomics, it has become clear that genetic effects are insufficient to account for differences in the incidence of RA (for instance, RA concordance in monozygotic twins is at best 15%). A gene–environment interaction, including its biological consequences, is therefore a more plausible explanation.