Beginning January 1, 2010, the Centers for Medicare and Medicaid Services (CMS)—formerly the Health Care Financing Administration (HCFA)—changed the rules eliminating consultation codes.1,2 The code was eliminated with this new policy by CMS and was not vetted through the Carrier Advisory Committee (CAC). According to a letter to CMS dated August 30, 2009, the American Medical Association (AMA) did not agree with this policy and urged CMS to work with the Current Procedural Terminology (CPT) Editorial Panel to explore alternatives.3
Research and Reactions
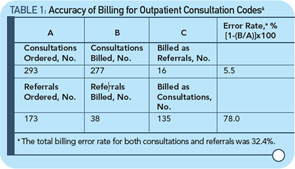
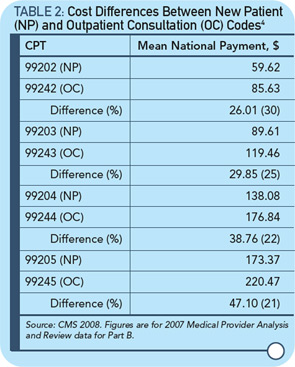
With this background, a recent article by Joel Shalowitz, MD, MBA, professor of health industry management at the Kellogg School of Management of Northwestern University in Evanston, Ill., defended the elimination of consultant codes.4 The objectives of the Shalowitz article were to describe the reasons for the codes, analyze the accuracy of the codes and project the financial repercussions of the elimination of consultations codes; the article also include recommendations for their continuation. The article involved the review of 500 requests for consultation and concluded that there were actually 293 consultations, 5% which were billed incorrectly; 173 were actually referrals of which 135 (78%) were incorrectly billed as consultations (see Table 1, above). The Health Insurance Portability and Accountability Act (HIPPA) was the reason patient-specific data was excluded from the analysis.4 In this study, there was no attempt to evaluate the quality of the consultations. The financial impact of changing the code was measured by correcting coding for consultation versus new patients codes, and showing how much money could be saved by paying less (see Table 2, below).4 The estimate for savings for Medicare was $534.5 million per year.
Dr. Shalowitz states that payment for services should be equalized, especially since the “consultant physicians are paid so much more than their primary care physicians for the same or less time spent with them.”4 In my opinion, this contention is wrong and Dr. Shalowitz has no data to support its validity. For cognitive consultative physicians, it is frustrating to read that the time spent on their consultations is “the same or less” than that of the primary care physician. I do not believe that this is true in rheumatology consultation.
Because of its designs, the article cannot assess the quality or impact of a consultation; rather, it focuses on coding and costs and not on care. As such, it can encourage the insurance company approach: Our costs will be less if we pay less. Importantly, in my view, the article uses the flawed interpretation of AMA semantics to distinguish between a referral and a consultation. I think that the approach to the patient can be virtually the same. If we call the encounter a new patient, however, we get paid less.
If CMS wishes to change payment schedule, I think that it should increase the new patient evaluation to the same reimbursement for the work and not use obfuscation to pay less. I think that the amount of effort during consultation is misinterpreted or ignored in a way that payors can use to decrease payments. Reduced reimbursement can directly impair the care of our patients. Regrettably, there is little in the Shalowitz article on the amount of work that was done by the physicians, the complexity of patients involved, and the quality of the work done. Shalowitz proposes that primary care physicians are unfairly treated by consultants. I strongly disagree. I believe that Dr. Shalowitz’s ideas foster unnecessary competition and discord between generalists and specialists and misconstrue the value of the consultation.
Shouldn’t Correct Count?
The best, most cost-effective diagnosis is the correct diagnosis. As a rheumatologist, I have saved patients, Medicare, and insurance companies countless dollars with the correct diagnosis, but nowhere in the Shalowitz article is the quality of the consultation considered. Many of our colleagues have commented on this article on the ACR Advocacy list serve. Paul Rochmis, MD, noted that the author’s statement that cognitive specialists “are paid so much more … or the same for less time spent with [patients]” is patently absurd (January 13, 2010). Where are the data supporting this statement? Does the author—and by extension, the editor—really think that the knowledge and experience in treating complex chronic illnesses will automatically flow from the medical specialist to the primary care physician with the 6% transfer of reimbursement? Chris Morris, MD, suggests Dr. Shalowitz does not understand the financial aspects of a private medical practice (January 13, 2010).
Dr. Shalowitz calculates the savings from this CMS rule change. If we rely on his data, this sum is $534.5 million dollars annually.1 For less than 1% savings, elimination of consultation codes will eliminate many Medicare patients’ access to specialists, as Dr. Rochmis noted on the ACR Advocacy list serve. Meanwhile, Tim Menke, deputy inspector general for investigations at the Department of Health and Human Services, estimates that Medicare fraud costs $60 billion a year and they only retrieve about $4 billion a year.5 Thus, instead of going after those who cheat Medicare, they go after physicians who have honestly worked hard for years for the care of their patients.
CMS and the insurers would do well to actually work with physicians who are on the front lines to develop health policy, and to avoid using only health industry management consultants. Do they call their advice “consultations”? The focus of payment policy should include the value of the correct diagnosis.
Dr. Goldman is a rheumatologist and president of Medical Quarters and chief of rheumatology at St. Joseph’s Hospital, both in Atlanta.
References
- CMS. CMS Manual System. Pub 100-20 One-Time Notification, Transmittal 615. Page 2. Published December 29, 2009. Available at: www.cms.hhs.gov/Transmittals/downloads/R615OTN.pdf. Accessed April 13, 2010.
- CMS. Summary of Policies in the 2010 Medicare Physician Fee Schedule (MPFS) and the Telehealth Originating Site Facility Fee Payment Amount – JA6756. Page 5. Published December 29, 2009. Available at: www.cms.hhs.gov/ContractorLearningResources/downloads/JA6756.pdf. Accessed April 13, 2010.
- Maves MD. Payment Policies Under the Physician Fee Schedule and Other Revisions to Part B for CY 2010; Proposed Rule; 74 Fed. Reg. 33,520 (July 13, 2009). August 31, 2009. Available at: www.ama-assn.org/ama1/pub/upload/mm/399/quality-pqri-letter-31aug2009.pdf. Accessed April 13, 2010.
- Shalowitz JI. Is it time to eliminate consultation codes? An analysis of impact and rationale. Arch Intern Med. 2010;170:14-17.
- Organized Crime Muscles In On Health Care. NPR Weekend Edition Saturday, January 16, 2010. Available at: www.npr.org/templates/player/mediaPlayer.html?action=1&t=1&islist=false&id=122645717&m=122645769. Accessed April 13, 2010.