Medication-related osteonecrosis of the jaw (MRONJ) is a condition that manifests as exposed, necrotic and non-healing jaw bone in patients who have been treated with bisphosphonates, denosumab, chemotherapeutic agents, anti-angiogenic drugs, tyrosine kinase inhibitors, thalidomide and steroids.1-4 These medications are administered via intravenous, subcutaneous and oral routes to manage osteopenia; osteoporosis; hypercalcemia of malignancy; bone metastases of tumors including lung, prostate and breast; and the lytic lesions of multiple myeloma.4
Pathogenesis & Treatment
In patients with MRONJ, the mandible is twice as likely to be involved as the maxilla.4 Three theories have been proposed relating to the pathogenesis of MRONJ:4-6
- Inhibition of osteoclastic function and increase in osteoclast apoptosis, which negatively affect bone healing and remodeling;
- Inflammation and infection secondary to biofilms; and
- Interruption of vascular supply leading to osteonecrosis.
MRONJ’s four stages, stage 0 to stage 3, reflect disease severity.4 Based on the staging and severity of the condition, MRONJ can be managed surgically and/or non-surgically.4
The non-surgical therapeutic approach includes pain control, antibacterial mouth rinses, systemic antibiotics, pentoxifylline and alpha-tocopherol. Surgical treatment includes debridement and sequestrectomy, resection and reconstruction.7
Risk Factors
Dentoalveolar surgery increases the risk of MRONJ, with tooth extraction being the most common precipitating factor.4 In a study conducted by Saad et al., tooth extraction as a predisposing event was reported by 61% of patients with MRONJ.8 Similarly, Hoff et al. identified dental extraction as a risk factor in 55% of patients in their cohort who developed MRONJ.9
The above-mentioned studies included patients treated with intravenous and subcutaneous bisphosphonates.
Hasegawa et al., in their multicenter, retrospective study, documented the incidence of post-extraction MRONJ in patients who received oral bisphosphonates as 1.7%.10
The best current estimate for the risk of developing MRONJ in patients on oral bisphosphonates after tooth extraction is 0.5%, whereas the risk for patients with cancer exposed to intravenous bisphosphonates ranges from 1.6–14.8%.4
A study conducted by Yamazaki et al. on patients receiving oral bisphosphonates for more than three years has demonstrated delayed recovery, with persistent bone exposure in the extraction sockets at four weeks, suggesting delayed epithelialization may be a cause of MRONJ.11
Bisphosphonates & Delayed Wound Healing
Several researchers have investigated the complex relationship between bisphosphonates and oral tissue toxicity. The results of these studies have revealed decreased oral epithelial cell migration and apoptosis, further causing delayed oral mucosal wound healing.12
In 2008, Landesberg et al. studied the effects of pamidronate on oral mucosal cells in a murine model. They found oral epithelial proliferation and wound healing were inhibited at pamidronate concentrations above 0.1 mmol/L, thereby contributing to the development of MRONJ through persistent exposure of the underlying bone.13
Scheper et al. assessed the apoptotic effects of zoledronic acid on human gingival fibroblast and keratinocyte cell lines using an in vitro model. They concluded that the direct contact of clinically relevant concentrations of zoledronic acid causes apoptosis of epithelial and fibroblast cells.14
Cell death and suppression of epithelial proliferation ultimately leads to mucosal thinning and breakdown, causing bone exposure and rapid microbial colonization, resulting in MRONJ.5,14 Therefore, it can be concluded that epithelialization and mucosal healing is an essential step in the management of MRONJ.
The prophylactic use of pentoxifylline & tocopherol two to three weeks prior to a dental extraction & continued therapy post extraction until the surgical site completely heals have been shown to reduce the incidence of MRONJ.
Autologous Platelet Concentrates
In 1998, Marx et al. reported the use of platelet-rich fibrin (PRF) as an accelerator in bone healing by influencing bone regeneration. PRF is obtained by sequestering and concentrating platelets by gradient density centrifugation.15 It is an autogenous source of platelet-derived growth factors, transforming growth factor β1 and transforming growth factor β2.15 Hence, PRF is responsible for enhancing the rate of wound healing and new bone formation. Since 1998, autologous platelet concentrates have gained popularity in oral and maxillofacial surgery. Its advantages and beneficial effects for improved soft tissue and bone healing have been validated in several other oral surgery procedures, as well.
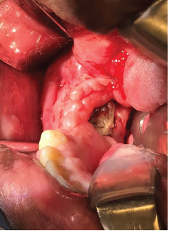
Exposed bone in the right mandible.
In 2007, Adornato et al. reported their experience using platelet-derived growth factors in managing refractory cases of MRONJ in 12 patients. They treated patients with a combination of the removal of necrotic bone and the application of PRF with resorbable collagen membrane.16 This therapy showed positive results, including complete wound healing, reduced treatment periods, less pain and improved quality of life.16
In 2012, Bocanegra-Perez et al. carried out a prospective descriptive study that included eight patients with a diagnosis of MRONJ. These patients were treated surgically with debridement of necrotic bone, followed by the application of leukocytes and PRF, and primary closure of the surgical site. The patients remained asymptomatic without dehiscence and evidence of exposed bone after an average 14-month follow-up period.17
PRF appears to be an accelerator of wound healing, preventing the occurrence of MRONJ in patients on bisphosphonate therapy undergoing tooth extraction.
In 2012, Mozzati et al. performed a case-control study on 176 patients requiring tooth extraction who were treated with intravenous zoledronic acid therapy. They divided the cohort into two groups: study and control groups. The study group, comprising 91 patients, was treated with plasma rich in growth factors (PRGF) post-extraction. The control group of 85 patients was not treated with PRGF post-extraction. They concluded that PRGF placement post-extraction reduces the risk of osteonecrosis of jaws.18
In 2017, Asaka et al. published their study, conducted at Hokkaido University Graduate School of Dental Medicine, Sapporo, Japan, of patients requiring tooth extraction who received oral bisphosphonate therapy for osteoporosis. A total of 102 patients met the inclusion criteria, which consisted of patients requiring tooth extraction who were on oral bisphosphonate therapy for osteoporosis or glucocorticoid-induced osteoporosis for more than one year.
The study compared a prospective cohort of patients treated with platelet-rich fibrin against historical controls.19 The PRF group consisted of 29 patients; the control group was made up of 73 patients.19 These patients had received oral bisphosphonate therapy for osteoporosis for an average of 32 months.19 Early epithelialization was confirmed in all PRF patients, and the prevalence of delayed recovery was significantly higher in the control group than in the PRF group.19 Thus, use of PRF may reduce the risk of delayed recovery in patients undergoing oral bisphosphonate therapy.
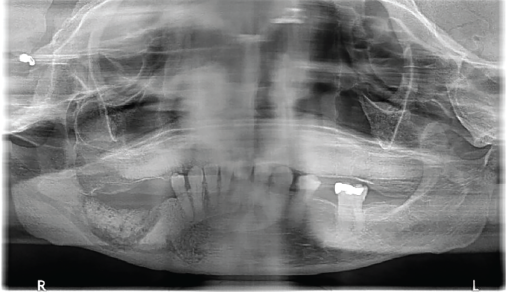
A panoramic radiograph shows sequestrum formation in the right mandible.
Pentoxifylline & Tocopherol
Pentoxifylline is a methylxanthine derivative that has been used for management of peripheral vascular diseases. It is known to decrease blood viscosity, improve erythrocyte flexibility and lower fibrinogen levels promoting fibrinolysis. Additionally, pentoxifylline reduces the plasma levels of tumor necrosis factor, interleukin (IL) 1 and IL-16, and decreases neutrophil activation, thereby enhancing anti-inflammatory and antioxidant effects.20 Tocopherol belongs to the vitamin E family and is used to decrease the risk of coronary artery disease. It is a potent oxygen radical scavenger with antioxidant and anti-inflammatory properties.21
Cell death & suppression of epithelial proliferation ultimately leads to mucosal thinning & breakdown, causing bone exposure & rapid microbial colonization, resulting in MRONJ.
Current literature suggests pentoxifylline in combination with tocopherol promotes both hard and soft tissue healing with minimal adverse effects and has been successfully used in patients with osteoradionecrosis (e.g., radiation-induced osteonecrosis of the jaw). This combination is used prophylactically to prevent osteonecrosis of jaws after dental extraction in patients with a history of radiation to the jaws. It is now being offered for the medical management of MRONJ.
The prophylactic use of pentoxifylline and tocopherol two to three weeks prior to a dental extraction and continued therapy post-extraction until the surgical site completely heals have been shown to reduce the incidence of MRONJ.22
 Pooja Gangwani, DDS, MPH, is an assistant professor of oral and maxillofacial surgery at the University of Rochester School of Medicine and Dentistry and Eastman Institute of Oral Health, Rochester, N.Y.
Pooja Gangwani, DDS, MPH, is an assistant professor of oral and maxillofacial surgery at the University of Rochester School of Medicine and Dentistry and Eastman Institute of Oral Health, Rochester, N.Y.
References
- Wutzl A, Pohl S, Sulzbacher I, et al. Factors influencing surgical treatment of bisphosphonate-related osteonecrosis of the jaws. Head Neck. 2012 Feb;34(2):194–200.
- Nicolatou-Galitis O, Schiodt M, Mendes RA, et al. Medication-related osteonecrosis of the jaw: Definition and best practice for prevention, diagnosis, and treatment. Oral Surg Oral Med Oral Pathol Oral Radiol. 2019 Feb;127(2):117–135.
- Patel V, Kelleher M, Sproat C, et al. New cancer therapies and jaw necrosis. Br Dent J. 2015 Sep 11;219(5):203–207.
- Ruggiero SL, Dodson TB, Fantasia J, et al. American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw—2014 update. J Oral Maxillofac Surg. 2014 Oct;72(10):1938–1956.
- Sedghizadeh PP, Kumar SKS, Gorur A, et al. Identification of microbial biofilms in osteonecrosis of the jaws secondary to bisphosphonate therapy. J Oral Maxillofac Surg. 2008 Apr;66(4):767–775.
- Sedghizadeh PP, Yooseph S, Fadrosh DW, et al. Metagenomic investigation of microbes and viruses in patients with jaw osteonecrosis associated with bisphosphonate therapy. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012 Dec;114(6):764–770.
- Fliefel R, Tröltzsch M, Kühnisch J, et al. Treatment strategies and outcomes of bisphosphonate-related osteonecrosis of the jaw (BRONJ) with characterization of patients: A systematic review. Int J Oral Maxillofac Surg. 2015 May;44(5):568–585.
- Saad F, Brown JE, Van Poznak C, et al. Incidence, risk factors, and outcomes of osteonecrosis of the jaw: Integrated analysis from three blinded active-controlled phase III trials in cancer patients with bone metastases. Ann Oncol. 2012 May;23(5):1341–1347.
- Hoff AO, Toth BB, Altundag K, et al. Frequency and risk factors associated with osteonecrosis of the jaw in cancer patients treated with intravenous bisphosphonates. J Bone Miner Res. 2008 Jun;23(6):826–836.
- Hasegawa T, Kawakita A, Ueda N, et al. A multicenter retrospective study of the risk factors associated with medication-related osteonecrosis of the jaw after tooth extraction in patients receiving oral bisphosphonate therapy: Can primary wound closure and a drug holiday really prevent MRONJ? Osteoporos Int. 2017 Aug;28(8):2465–2473.
- Yamazaki T, Yamori M, Ishizaki T, et al. Increased incidence of osteonecrosis of the jaw after tooth extraction in patients treated with bisphosphonates: a cohort study. Int J Oral Maxillofac Surg. 2012 Nov;41(11):1397–1403.
- Soydan SS, Uckan S. Management of bisphosphonate-related osteonecrosis of the jaw with a platelet-rich fibrin membrane: Technical report. J Oral Maxillofac Surg. 2014 Feb;72(2):322–326.
- Landesberg R, Cozin M, Cremers S, et al. Inhibition of oral mucosal cell wound healing by bisphosphonates. J Oral Maxillofac Surg. 2008 May;66(5):839–847.
- Scheper MA, Badros A, Chaisuparat R, et al. Effect of zoledronic acid on oral fibroblasts and epithelial cells: A potential mechanism of bisphosphonate-associated osteonecrosis. Br J Haematol. 2009 Mar;144(5):667–676.
- Marx RE, Carlson ER, Eichstaedt RM, et al. Platelet-rich plasma: Growth factor enhancement for bone grafts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998 Jun;85(6):638–646.
- Adornato MC, Morcos I, Rozanski J. The treatment of bisphosphonate-associated osteonecrosis of the jaws with bone resection and autologous platelet-derived growth factors. J Am Dent Assoc. 2007 Jul;138(7):971–977.
- Bocanegra-Pérez S, Vicente-Barrero M, Knezevic M, et al. Use of platelet-rich plasma in the treatment of bisphosphonate-related osteonecrosis of the jaw. Int J Oral Maxillofac Surg. 2012 Nov;41(11):1410–1415.
- Mozzati M, Arata V, Gallesio G. Tooth extraction in patients on zoledronic acid therapy. Oral Oncology. 2012 Sep;48(9):817–821.
- Asaka T, Ohga N, Yamazaki Y, et al. Platelet-rich fibrin may reduce the risk of delayed recovery in tooth-extracted patients undergoing oral bisphosphonate therapy: A trial study. Clin Oral Investig. 2017 Sep;21(7):2165–2172.
- McCarty MF, O’Keefe JH, DiNicolantonio JJ. Pentoxifylline for vascular health: A brief review of the literature. Open Heart. 2016 Feb 8;3(1):e000365.
- Jiang Q. Natural forms of vitamin E: Metabolism, antioxidant, and anti-inflammatory activities and their role in disease prevention and therapy. Free Radic Biol Med. 2014 Jul;72:76–90.
- Heifetz-Li JJ, Abdelsamie S, Campbell CB, et al. Systematic review of the use of pentoxifylline and tocopherol for the treatment of medication-related osteonecrosis of the jaw. Oral Surg Oral Med Oral Pathol Oral Radiol. 2019 Nov;128(5):491–497.e2.


