 How to Manage Organ Manifestations of Sarcoidosis & Help Patients
How to Manage Organ Manifestations of Sarcoidosis & Help Patients
EULAR 2024 (VIENNA)—Sarcoidosis: It’s a multi-system inflammatory disease that triggers many referrals to rheumatology—and perhaps just as many groans from the rheumatologists who receive those referrals. But why? After all, who better to manage a multi-system inflammatory disease than a rheumatologist?1
At EULAR 2024, Arthur M.F. Yee, MD, PhD, director, Hospital for Special Surgery Sarcoidosis Collaborative, HSS/Weill Cornell Medicine, New York, championed and encouraged the rheumatologist’s involvement in the care of patients with sarcoidosis. It was a great session, and quite frankly, a peptalk that many of us—myself included—needed to hear.
Sarcoidosis Needs a Rheumatologist
Dr. Yee
Dr. Yee opened his session with a call to action.
“When I was first asked to speak, the title I was given was ‘Sarcoidosis: Joint, Bone and Muscles,’ and I badgered the organizers to let me change it,” he said. “I changed it to ‘Sarcoidosis: (Not Just) Bone, Joint and Muscles’ because I think the role of rheumatologists has been understated. We need to take a stronger role in taking care of these patients as individuals and as a community.”
Dr. Yee shared two timelines depicting when certain medications, including prednisone, chloroquine, methotrexate, infliximab and tofacitinib, should be introduced for the treatment of rheumatoid arthritis (RA) and sarcoidosis (see Figure 1). “As you can see, in every case, the use of medications for RA precedes those for sarcoidosis by many years,” he said. “So I would wager a guess that many of the medications we are talking about outside right now in poster form may have applicability to sarcoidosis going forward.”
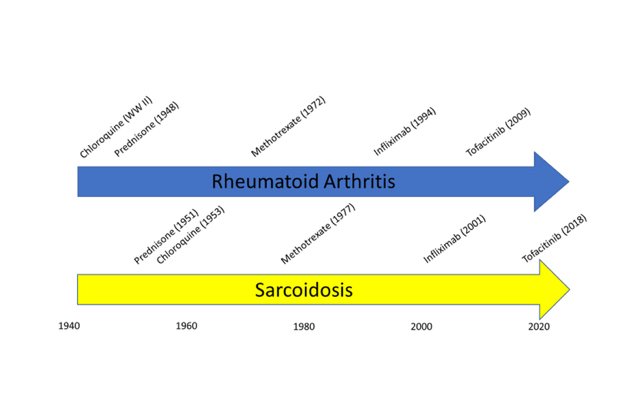
Figure 1: Timeline comparing when medications were introduced for RA vs. sarcoid.
Why aren’t rheumatologists more interested in sarcoidosis? The condition is similar to so many diseases we don’t hesitate to manage, such as systemic lupus erythematosus. Like lupus, sarcoidosis is a multi-system disease of immunologic dysregulation that has hallmark laboratory and pathologic findings. It’s a clinical diagnosis with variable phenotypes, courses and tempo, with both inflammatory and non-inflammatory features. It has acute and long-term morbidities, immunomodulatory treatment paradigms and racial and sex disparities. Further, lupus and sarcoidosis have a similar prevalence in the U.S. Several diseases, such as vasculitis and inflammatory myositis, are rarer.
“You’d think that if we’re comfortable with [managing] lupus, we’d also be comfortable with [managing] sarcoidosis. We should be taking a stronger role. There are many reasons we haven’t, but we should get over ourselves,” he said.
Referrals to Rheumatology
Any organ can be affected in this condition, and when multiple organs are affected all at once and no one else can figure it out, a rheumatologist is who gets the call.
“The most bizarre case [of sarcoidosis] I ever saw was in the prostate,” Dr. Yee said.
Dr. Yee and his colleagues are currently conducting a study to better understand rheumatology referral queries. “By and large, these patients are referred to us for medication management. But the question we’re being asked is, ‘What medications will actually work for these patients?’—not what drug to start. We are being asked to adjust therapy, not initiate it. This suggests that [the patients with] sarcoidosis we see are more complicated and more difficult to manage,” he said.
Highlights
Every sarcoidosis manifestation has a broad differential. Example: A multi-system illness should prompt consideration of Sjögren’s disease, tuberculosis, syphilis and lymphoma, among others.
“The bottom line is that there are many different conditions you need to think about. [Studying up on] sarcoidosis is a great way to prepare for the internal medicine boards because you end up learning everything over and over again,” Dr. Yee said.
Interestingly, Dr. Yee noted that—in his opinion—perhaps the most important rheumatic manifestation of sarcoidosis has nothing to do with direct inflammation itself, but rather is a consequence of inflammation: granulomas. Granulomas can convert 25-hydroxy-vitamin-D3 (i.e., the vitamin D level measured on routine bloodwork) into 1,25-dihydroxy-vitamin-D3 in a parathyroid hormone (PTH) independent manner. Thus, 25-hydroxy-vitamin-D3 levels may be low, but 1,25-dihydroxy-vitamin-D3 levels may actually be high in patients. This is a problem because 1,25-dihydroxyvitamin-D3 is the active hormone and too much of it can cause such issues as hypercalcemia, hypercalciuria, nephrolithiasis and osteoporosis.2
“I check 1,25-dihydroxy-vitamin-D3 levels in all [patients with] sarcoidosis because you can’t otherwise tell if they’re [vitamin D] deficient or not, and you may be doing harm if trying to replete someone inappropriately,” he said.
Post-Diagnosis Screening
In 2020, the American Thoracic Society published a clinical practice guideline for the diagnosis and detection of sarcoidosis.3 This document included screening recommendations for patients newly diagnosed with sarcoidosis regardless of clinical manifestations of disease:
- Complete blood count;
- Comprehensive metabolic panel;
- 25-hydroxy-vitamin-D3, 1-25-dihydroxy-vitamin-D3 and calcium levels;
- Electrocardiogram; and
- Ophthalmologic examination.
“Of note, these [recommendations] don’t mention chest X-ray or pulmonary function tests because they take the [pulmonolgist’s] point of view, and pulmonologists automatically order these for their patients. So remember to include these [tests] too, [because] pulmonary sarcoidosis can be asymptomatic,” Dr. Yee said.
‘You’d think that if we’re comfortable with [managing] lupus, we’d also be comfortable with sarcoidosis. We should be taking a stronger role [with this condition].’ —Dr. Yee
Treatment
Corticosteroids and repository adrenocorticotropic hormone (ACTH) are the only medications approved by the U.S. Food & Drug Administration for the treatment of sarcoidosis. “However, [corticosteroids and ACTH] are my first line of defense and my last resort at the same time,” Dr. Yee said.
Conventional anti-metabolites are frequently used off label with methotrexate, azathioprine, mycophenolate mofetil and leflunomide.4 Hydroxychloroquine, thalidomide, cyclosporine and cyclophosphamide are used less commonly.
Tumor necrosis factor (TNF) inhibitors have proven effective. Infliximab has been shown to improve both pulmonary and extra-pulmonary disease manifestations.5,6 “The bottom line is that infliximab and adalimumab work [for sarcoidosis], but etanercept doesn’t; this is probably[for] the same reason it doesn’t work in Crohn’s disease. As a soluble receptor, [etanercept] cannot get to the granuloma,” Dr. Yee said.
The heart: What about patients with cardiac sarcoidosis? In 2003, the ATTACH trial studied the use of infliximab for the treatment of patients with non-sarcoidosis heart failure with negative and detrimental results.7 In patients receiving high-dose infliximab (i.e., 10 mg/kg), the combined risk of death from any cause or hospitalization for heart failure was increased through 28 weeks compared with patients not on infliximab or those on low-dose infliximab (5 mg/kg). This finding led to the contraindication for TNF inhibitors in patients with reduced ejection fraction, of which we are all aware.
“For many years, the cardiologists at my institution fought back at me when we had a [patient with] cardiac sarcoidosis, and I wanted to give infliximab. Fortunately, this issue has now been settled. In 2020, Baker et al. showed absolutely no deterioration of cardiac function in patients given infliximab for cardiac sarcoidosis and a reduction in steroid dependence,” Dr. Yee said.8
Of note, recent studies also show promise for tofacitinib for the treatment of sarcoidosis.9
Stopping Medications
When it comes to stopping medications in patients with sarcoidosis, data come from retrospective studies.
Dr. Yee identified eight patients in his clinic who could come off TNF inhibitor treatment after establishing complete remission.10 Before TNF inhibitors were stopped, all eight patients remained stable off systemic corticosteroid therapy for at least a year. So, he said, “the sustained capacity to remain off corticosteroids during TNF inhibitor therapy may be a favorable prognostic indicator for maintained disease remission.” 10
Take-Home Points
In summary, sarcoidosis is a fascinating multi-system inflammatory disease that rheumatologists are uniquely positioned to treat. It’s time for us to step up to the plate and collaborate with our colleagues on multi-disciplinary teams to better care for these patients.
Samantha C. Shapiro, MD, is a clinician educator who is passionate about the care and education of rheumatology patients. She writes for both medical and lay audiences and practices telerheumatology.
References
- Yee AMF. Sarcoidosis: Rheumatology perspective. Best Pract Res Clin Rheumatol. 2016 Apr;30(2):334–356.
- Fuss M, Pepersack T, Gillet C, et al. Calcium and vitamin D metabolism in granulomatous diseases. Clin Rheumatol. 1992 Mar;11(1):28–36.
- Crouser ED, Maier LA, Baughman RP, et al. Diagnosis and detection of sarcoidosis an official American Thoracic Society Clinical Practice guideline. Am J Respir Crit Care Med. 2020 Apr 15;201(8):e26–e51.
- Baughman RP, Winget DB, Lower EE. Methotrexate is steroid sparing in acute sarcoidosis: Results of a double blind, randomized trial. Sarcoidosis Vasc Diffuse Lung Dis. 2000 Mar;17(1):60–66.
- Judson MA, Baughman RP, Costabel U, et al. Efficacy of infliximab in extrapulmonary sarcoidosis: Results from a randomised trial. Eur Respir J. 2008 Jun;31(6):1189–1196.
- Baughman RP, Drent M, Kavuru M, et al. Infliximab therapy in patients with chronic sarcoidosis and pulmonary involvement. Am J Respir Crit Care Med. 2006 Oct 1;174(7):795–802.
- Chung ES, Packer M, Lo KH, et al. Randomized, double-blind, placebo-controlled, pilot trial of infliximab, a chimeric monoclonal antibody to tumor necrosis factor-α, in patients with moderate-to-severe heart failure: Results of the anti-TNF therapy against congestive heart failure (ATTACH) trial. Circulation. 2003 Jul 1;107(25):3133–3140.
- Baker MC, Sheth K, Witteles R, et al. TNF-alpha inhibition for the treatment of cardiac sarcoidosis. Semin Arthritis Rheum. 2020 Jun;50(3):546–552.
- Damsky W, Wang A, Kim DJ, et al. Inhibition of type 1 immunity with tofacitinib is associated with marked improvement in longstanding sarcoidosis. Nat Commun. 2022 Jun 6;13(1):3140.
- Yee AMF. Durable medication-free remission of sarcoidosis following discontinuation of anti-tumor necrosis factor-α therapy. Respir Med. 2023 Jan:206:107055.
