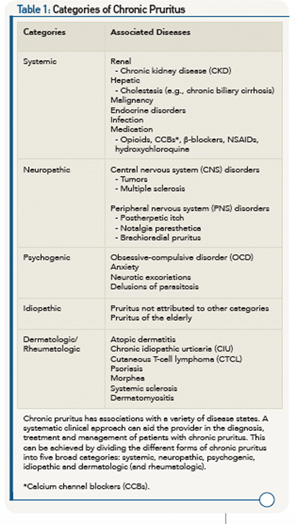
Neuropathic Itch
In contrast to systemic chronic itch, which is likely mediated by circulating factors or pruritogens, neuropathic itch derives from pathology along the afferent nervous system.41 The nervous system can be activated either centrally or peripherally. Tumors or degenerative diseases of the CNS (e.g., multiple sclerosis) can lead to centrally mediated mechanisms of pruritus.42
More commonly, neuropathic itch is triggered within the PNS. For example, viral damage to peripheral neurons is thought to mediate postherpetic itch in a manner similar to postherpetic neuralgia.43,44
Another example of peripherally mediated pruritus includes notalgia paresthetica, which presents as chronic, localized itch most often on the central back. Although the exact etiology remains unknown for notalgia paresthetica, it has been theorized that sensory nerve entrapment, involving the posterior rami of the T2 to T6 nerve root, occurs due to degenerative changes in the vertebrae.45 In a similar fashion, brachioradial pruritus manifests as chronic, intermittent pruritus along the arms and is thought to be caused by nerve impingement along the cervical spine.46
For the treatment of neuropathic itch, a variety of neuromodulators are employed empirically. For example, topical capsaicin has been shown to improve symptoms in notalgia parasthetica.47 The mechanism of action of capsaicin is activation of the sensory nerve receptor TRPV1, which leads to depletion of substance P and neuronal desensitization.48 For postherpetic itch and brachioradial pruritus, gabapentin has demonstrated efficacy as well.49 Its mechanism of action is believed to be via binding of the α2δ1 subunit of voltage-dependent calcium channels in dorsal horn postsynaptic cells.50
Other treatments attempted in neuropathic itch include oxcarbazepine, botulinum toxin or, in the case of nerve entrapment, physical therapy and/or surgery.
Psychogenic Itch
Psychogenic pruritus is a diagnosis of exclusion that presents in association with an underlying psychiatric disorder, such as obsessive-compulsive disorder (OCD), anxiety disorder or substance abuse.41 Associated conditions include neurotic excoriations or excoriation disorder, which is now recognized in the DSM-V manual.51 These diseases are strongly influenced by variations in life events and stress. Typical findings include excoriations, erosions, ulcers and scarring in areas of the body that can be easily manipulated by the patient, such as the extensor surfaces and face.52 Delusions of parasitosis, a relatively uncommon psychiatric condition, presents with the patient having a fixed belief that he or she has been infested with arthropods or parasites.53 The patient suffers from these delusions and consciously produces self-inflicted wounds as a result.