
Studio_G / shutterstock.com
The evaluation and management (E/M) code set in the American Medical Association’s Current Procedural Terminology (CPT) book lists descriptors, as well as typical times for patient visits. These times are averages of how long it takes a physician to complete all components of a visit at each level. Because the specific times identified in the CPT book are averages, they represent a range of times that may be higher or lower depending on actual clinical circumstances from visit to visit. It’s important to understand that time is only a contributing factor in determining which level of E/M to report.
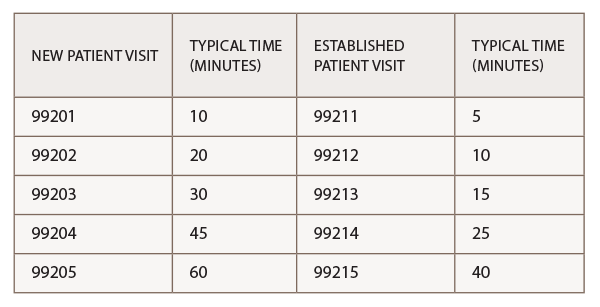
The key components of history, examination and medical decision making are usually used to determine an E/M level of service, if a provider ends up spending more than 50% of the total visit counseling and coordinating care, then time can be used as the key factor in determining the E/M level to bill for that service. Per the CPT, typical times for new and established office visits are:
When coding on the basis of time in the outpatient setting, providers can count only face-to-face time with the patient or family. This face-to-face time includes not only the time spent counseling, but also the time associated with any history, exam or medical decision making performed. Time spent reviewing records, talking with other providers and documenting the encounter without the patient or family present cannot be considered. It is not unusual for rheumatologists to spend significant time during an office visit reviewing new and/or existing problems, modifying medications, counseling and coordinating care. To determine whether to code for time as the key factor, the following questions must be answered:
- How much time did I spend either counseling or coordinating care for the patient?
- How much time did I spend in total for the visit (including time spent providing key components and time spent counseling and/or coordinating care)?
Example
A 62-year-old male patient returns to the office for a follow-up visit for his gout. The history of present illness is extended, an expanded problem focus examination is conducted, and medical decision making is of low complexity, which would normally be coded as a level 3 visit (99213). But the total time for the visit is 30 minutes, and more than 50% of that time is spent on counseling the patient on a diet and exercise plan.
Because time and the discussion were documented and more than 50% of the visit was spent with the patient face to face, time is the key factor in determining the level of this visit. CPT states that an established patient level 4 visit is typically 25 minutes long; this visit was 30 minutes long, which qualifies the visit to be coded 99214.
In every case, it’s imperative to document the extent of the counseling/coordination of care in the patient’s medical record.
Prolonged Time
In addition to using time as the qualifying factor for a higher E/M level, CPT also has face-to-face and non-face-to-face prolonged time codes that can be billed, in addition to an E/M code if time spent extends at least 30 minutes beyond the typical amount of time allotted for that visit. The CPT codes for face-to-face prolonged visits are 99354–99357, and these add-on codes cannot be billed separately without an E/M code.
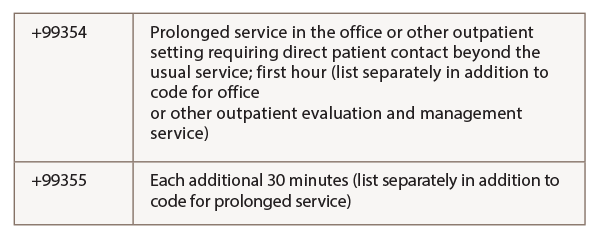
CPT defines 99354 as “prolonged physician service in the office or other outpatient setting requiring direct (face-to-face) patient contact beyond the usual service; first hour.” For example, an established patient is seen with a level 5 office visit—typically 40 minutes long—but an extensive workup is performed due to multiple diagnoses, which requires the physician spend an extra 20 minutes with the patient. In this case, it is appropriate to code the claim as 99215 and 99354.
The non-face-to-face prolonged service codes without direct patient contact are 99358 and 99359. CPT allows codes 99358 and 99359 to be used when “a physician provides prolonged service not involving direct (face-to-face) care that is beyond the usual non–face-to-face component of physician service time.” These codes are to be reported in relation to other E/M services at any level, but may be reported for a different date of service than that of the primary E/M service they are related to.
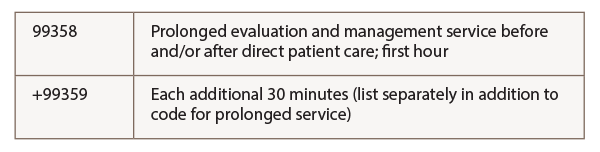
For example, if a physician spends an hour extensively reviewing a new patient’s medical records prior to their office visit, the time spent would be documented and included in the patient’s medical record during their scheduled visit. CPT codes 992XX and 99358 would be billed. For each additional 30 minutes over the first initial hour of the prolonged service, CPT code +99359 should be used. Note that 99359 is an add-on code and cannot be billed separately without 99358.
For more information on documenting the use of time, download a copy of the ACR’s Rheumatology Coding Manual, review the E/M services guidelines in the current CPT manual, or read Medicare’s Documentation Guidelines for E/M Services at www.cms.gov.
Time plays an important role in the selection of the most appropriate code for services. Understanding the rules related to time-based coding will help in obtaining proper payment as time is a key element necessary to help meet the appropriate treatment goals for patients. If you have any questions, contact Melesia Tillman CPC-I, CRCH, CHA, at [email protected] or 404-633-3777 x820.

