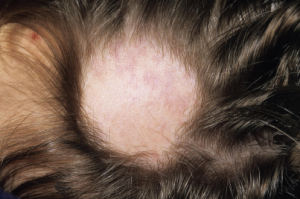
Hair loss is commonly seen in lupus patients, but not all alopecia types are the same.
Dr P. Marazzi/Science Source
SAN DIEGO—Rheumatologists who treat lupus patients gleaned tips on diagnosis and management of renal disease, painful neuropathies and alopecia at a “Curbside Consults” session held Nov. 6 at the ACR/ARHP Annual Meeting in San Diego.
Membranous Lupus Nephritis
Patients with refractory membranous lupus nephritis (MLN), or Class V lupus nephritis, face “significant morbidity, most of which is related to nephrotic syndrome and hypo-albuminemia,” said Ellen M. Ginzler, MD, MPH, distinguished teaching professor of medicine and chief of rheumatology at SUNY Downstate Medical Center in Brooklyn, N.Y. About 20% of lupus nephritis patients have MLN, and 10% may progress to end-stage renal disease after 10 years.1
“So this is not a trivial problem. It’s important to think about possible consequences when you choose initial treatment,” including women who wish to become pregnant later, she said. Current ACR guidelines recommend pulse prednisone with a range of 0.5 to 1 mg/kg a day and immunosuppressant therapy, but “the question is which immunosuppressant drug to use?”2 Both the ACR and EULAR guidelines suggest mycophenolate mofetil (MMF), but intravenous cyclophosphamide is another option.3 She shared a case of a nulliparous, 32-year-old woman with MLN who started on 30 mg of prednisone and 3 g of MMF daily, and Dr. Ginzler suggested that African American and Afro-Caribbean patients may do better on the higher range of the recommended dose.
Although her patient’s blood pressure was normal, Dr. Ginzler also prescribed losartan, an angiotensin receptor blocker (ARB). ARBs and angiotensin-converting enzyme inhibitors “may lower proteinuria, but give you a false sense of security, because what they do is decrease renal blood flow, not really affecting the glomerular pathology” in MLN patients, she said. When her patient later wanted to conceive, she switched from MMF to azathioprine, although it can elevate risk of renal flare in some patients, said Dr. Ginzler.
“Unfortunately, my patient was one of them, and eight months later, she had a flare, and again had hypo-albuminemia and significant nephrotic syndrome,” she said. Renal biopsy confirmed that she still had pure MLN, so she restarted induction therapy with a slightly higher prednisone dose. She redeveloped leg edema, still had proteinuria, and was later confirmed to have renal vein thrombosis. She started anticoagulation therapy, and then Dr. Ginzler and her colleagues chose to also start cyclosporin, a calcineurin inhibitor, based on current guidelines. Trials of calcineurin inhibitors are few, small, mainly anecdotal and do not focus on patients with pure MLN, she said. One meta-analysis focused on pure MLN patients suggests rituximab is another option, with 40% of patients achieving complete and 27% achieving partial response.4
Two new interventional clinical trials are now recruiting patients with pure MLN, “so there is some hope on the horizon for new therapies for patients with refractory nephrotic syndrome and proteinuria,” said Dr. Ginzler.
Small-Fiber Neuropathies
When his 44-year-old patient with systemic lupus erythematosus (SLE) used highly poetic language to describe widespread pain, her colorful metaphors pointed to a small-fiber neuropathy (SFN) diagnosis, said Julius Birnbaum, MD, MHS, assistant professor of medicine at the Johns Hopkins University School of Medicine in Baltimore.
“She described a sensation of caterpillars with sharp claws crawling up her arms and marching up her neck, hot vats of oil being poured over her thighs, and that her arms and legs ached when she put on any clothes,” he said.
SFNs are sensory, uniformly painful neuropathies that target predominantly unmyelinated C-fiber nerves. Clinical features include burning and lancinating pain, paroxysmal pain and/or intense allodynic pain, he said. SFNs may affect patients with SLE, Sjögren’s syndrome, rheumatoid arthritis, viral and fungal infections, celiac disease, sarcoidosis, scleroderma or diabetes, and it has also been associated with TNF-inhibitor therapy in some patients.5
Look for small fiber deficits on examination: a decrease in pain to pinprick or temperature, and sometimes an increased pain to pinprick hyperalgesia, he said. Nerve conduction studies will be normal, because these only assess the integrity of large-fiber nerves.
Punch skin biopsy on either the proximal thigh or distal leg is the most effective diagnostic tool.6 Look for decreased unmyelinated nerves in the epidermal layer, or “decreased inter-epidermal nerve fiber density” on the pathology report, he said.7 “Punch skin biopsy is easy to do, takes only 15–20 minutes and is minimally invasive. Sensitivity, depending on the underlying neuropathic syndrome, is 60–90% with a specificity above 95%.” Skin biopsy also helps distinguish between length-dependent and non-length-dependent forms of SFN.
‘Whatever treatments are on the horizon, don’t be afraid to tell patients that they have a powerfully painful disorder that will get better, but slowly.’ —Julius Birnbaum, MD, MHS
Patients’ hands may be affected more than their feet, and some have whole-body burning pain, said Dr. Birnbaum. Skin biopsy helps distinguish which neural targets, such as the dorsal root ganglia or the axon, are the sites where pain developed. Quantitative sensory testing (QST) is another method to diagnose SFN, although a patient’s descriptions of the pain are often the best guide.
SFN treatment is challenging, and may require several agents or a combination, said Dr. Birnbaum. Gabapentin, nortriptyline, venlafaxine XR and opioids may be useful, as well as topical agents, such as capsaicin or lidocaine.
“Whatever treatments are on the horizon, don’t be afraid to tell patients that they have a powerfully painful disorder that will get better, but slowly, and that there’s no guarantee that the first, second or even third agent that we use will help,” he said. “I know that sounds negative, but I find that it resonates with patients, because they’ve likely been down this road before. Be bold and creative, and try polysymptomatic approaches.”
Alopecia
Hair loss is commonly seen in lupus patients, but not all alopecia types are the same, said Victoria P. Werth, MD, professor of dermatology at the Hospital of the University of Pennsylvania in Philadelphia. Rheumatologists may encounter lupus->specific alopecia, lupus-nonspecific alopecia or alopecia unrelated to their lupus at all. Alopecia is included in the new ACR/EULAR classification criteria for SLE.
“Lupus-specific alopecia is something I think we’re all very familiar with in these patients. They usually have underlying erythema and scale, and it’s associated with lesions that are due to discoid lupus, sub-acute cutaneous lupus or acute SLE,” said Dr. Werth. Patients may have dispigmentation, permanent hair loss and follicular plugging.
Lupus-nonspecific alopecia is non-scarring. These patients may have “lupus hairs,” or coarse, dry, fragile, very short hairs on the scalp along the forehead. “This can include diffuse areas of non-scarring alopecia which waxes and wanes with systemic disease activity, and can be a manifestation of the telogen effluvium [temporary hair loss] that is not specific to lupus, but we see plenty of it in our SLE patients.”
About 10% of SLE patients have alopecia arreata unrelated to their disease. These patients have circular, totally hairless patches, but no erythema or scale. Their telogen effluvium may happen postpartum, after surgery or due to stress, she said. Some SLE patients also have androgenic alopecia, or typical male- or female-pattern baldness.
Patients with subacute cutaneous lupus or acute SLE may have a temporary hair loss followed by regrowth later, she said. Using a magnifying lens or dermatoscope, loss of follicular ostia can be seen, which means the hair loss is permanent, she said.
Biopsy on a horizontal section of the scalp is one way to diagnose the alopecia type. “Look for the changes of lupus in the skin, look at the different follicles to see what happened to them, and check for follicular scarring,” which means hair is not regrowing and is likely telogen-related, she said.
Incidence is unclear, but lupus-nonspecific alopecia may affect up to 40% of SLE patients. In these cases, hair often regrows when disease activity is controlled. These patients may have short, thin hair along with typical lupus flare symptoms. Medication may also cause this temporary hair loss.
In lupus patients with alopecia arreata, a gentle hair pull test may reveal dystrophic androgen hairs, and a dermoscopy often shows “exclamation point” hairs. Biopsy of these patients may show mononuclear cell infiltrate and mucin deposition, as well as inflammatory cells around the hair follicle that look like swarms of bees, she said. Direct immunofluorescence may show signs of inflammation.
Patients with tightly pulled hairstyles may also have traction alopecia, she said. Lupus patients with alopecia should avoid sun exposure and wear hats, said Dr. Werth. “If you can see through the hat, it’s not good enough for sun protection,” she added. Treatments include topical and intralesional steroids, topical tacrolimus or pimecrolimus, antimalarials, methotrexate and, in severe cases, thalidomide or lenalidomide. Hair weaves or hairpieces help conceal areas of permanent hair loss, she concluded.
Susan Bernstein is a freelance journalist based in Atlanta.
References
- Okpechi IG, Ayodele OE, Jones ESW, et al. Outcomes of patients with membranous lupus nephritis in Cape Town, South Africa. Nephrol Dial Transplant. 2012 May;27(9):3509–3515.
- Hahn BH, McMahon MA, Wilkinson A, et al. American College of Rheumatology guidelines for the screening, treatment and management of lupus nephritis. Arth Care Res. 2012 Jun;64(6):797–808.
- Bertsias GK, Tektonidou M, Amoura Z, et al. Joint European League Against Rheumatism and European Renal Association-European Dialysis and Transplant Association recommendations for the management of adult and paediatric lupus nephritis. Ann Rheum Dis. 2012 Nov;71(11):1771–1782.
- Wiedenbusch M, Rommele C, Schrottle A, et al. Beyond the LUNAR trial. Efficacy of rituximab on refractory lupus nephritis. Nephrol Dial Transplant. 2013 Jan;28(1):106–111.
- Birnbaum J, Bingham CO III. Non-length-dependent and length-dependent small-fiber neuropathies associated with tumor necrosis factor (TNF)-inhibitor therapy in patients with rheumatoid arthritis: Expanding the spectrum of neurological disease associated with TNF-inhibitors. Semin Arthritis Rheum. 2014 Apr;43(5):638–647.
- Sommer C, Lauria G. Skin biopsy in the management of peripheral neuropathy. Lancet Neurol. 2007 Jul;6(7):632–642.
- Chai J, Herrmann DN, Stanton M, et al. Painful small fiber neuropathy in Sjogren syndrome. Neurology. 2005 Sep;65(6):925–927.
- Werth VP, White WL, Sanchez MR, et al. Incidence of alopecia arreata in lupus erythematosus. Arch Dermatol. 1992 Mar;128(3):368–371.

