The Lupus-Gut Connection
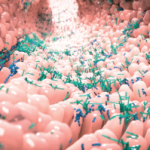
Dr. Silverman says his team is cloning bacteria from the intestines of lupus patients. “It is amazing to be able to do whole-gene sequencing on these bacteria, learn their secrets and determine how they contribute to illness,” he says. “We are also looking at patients at multiple time points, asking, ‘Do patients remain stable with the same microbiome over time? How is this related to the immune system?’ Our goal is to be able to obtain a more accurate diagnosis—and to do so in a timely fashion.”
The next steps are to confirm the findings from this study in other lupus populations. “Ideally, this kind of testing can tell us whether someone is likely to progress to kidney disease,” he says. “It is important that we look at how to shift the microbiome away from bad bacteria; this may involve fecal transplants. While, thus far, this treatment has been successful in many patients with a bowel disease … we are not ready to attempt it in patients with SLE.”
The takeaway for practicing rheumatologists? “This work can help bring hope to patients that perhaps there are simple things we can do to improve their conditions,” Dr. Silverman says. “In the future, this may lead to therapies that would stand in great contrast to the current standard of care for lupus nephritis, which involves escalating medications that suppress the immune system—cancer therapy that basically kills the immune system.”
Elizabeth Hofheinz, MPH, MEd, is a freelance medical editor and writer based in the greater New Orleans area.
Reference
- Azzouz D, Omarbekova A, Heguy A, et al. Lupus nephritis is linked to disease-activity associated expansions and immunity to a gut commensal. Ann Rheum Dis. 2019 Jul;78(7):947–956.