In ancient Roman mythology, the two-faced Roman God Janus presided over all beginnings and transitions. On November 6, 2012, the U.S. Food and Drug Administration (FDA) approval of the first Janus kinase (JAK) inhibitor, tofacitinib, for treatment of rheumatoid arthritis (RA) heralded the advent of kinase inhibitors in the therapeutics of rheumatic diseases. Despite the advances in treatment of RA over the last two decades by the use of cytokine and target cell inhibitors, a significant percentage of RA patients either do not respond or lose their response to therapy. The pathophysiology of rheumatoid arthritis is dependent on the activation of both the innate and adaptive immune systems. The cells that comprise the immune system utilize kinases as the gatekeepers to determine how they should respond to external stimuli such as antigens, cytokines, and immune complexes. The use of new small molecule inhibitors against cytoplasmic kinases such as the JAK family, splenic tyrosine kinase (SYK), or mitogen-activated phosphokinase p38 (p38MAPK) will alter the resulting dysregulated immune systems in different ways and hopefully further promote our understanding of its complexities.
Small Molecule Mechanism of Action
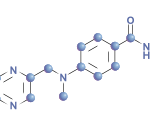
In addition to the newly released tofacitinib, at least three other JAK inhibitors are currently in phase II studies for treatment of RA, psoriasis, and inflammatory bowel disease (see Table 1). The mechanism of action of these agents is unique compared to currently available therapeutic modalities by its effect on the intracellular signaling apparatus comprising the JAK family network used by inflammatory cytokines and other growth factors. Following binding of cytokines or growth factors to their respective receptor, JAKs phosphorylate and activate members of the signal transducer and activator of gene transcription (STAT) family. Inflammatory cytokines such as interleukin (IL) 6, IL-2, and IL-12/IL-23 are dependent on the Janus family of kinases. The JAK family is composed of four tyrosine kinases. JAK-1, JAK-2, and TYK2 are expressed ubiquitously, but JAK 3 is limited to lymphoid tissues.1 All JAKs possess two similar phosphate-transferring domains, one with actual kinase activity and the pseudokinase domain, which negatively regulates the kinase activity of the first.2 This dual regulatory function led to the origin of its name, JAK, taken from the mythological god Janus represented by two faces and often present over doorways symbolizing transitions. The JAK-STAT interaction is responsible for the signal transduction of over 50 members of the 4-helix bundle cytokine family, including interferons and growth factors such as leptin, prolactin, GM-CSF, and erythropoietin (EPO).
Future studies of additional kinases will help elicit a better understanding of the complex coding mechanisms of regulation of both innate and adaptive immune systems.
Spotlight on Tofacitinib
Tofacitinib was approved for use in patients with moderate to severe rheumatoid arthritis who have had an inadequate response or intolerance to methotrexate (MTX) as monotherapy or with other nonbiological disease-modifying antirheumatic drugs (DMARDs).3 Its principal target is JAK1/JAK3. The treatment results in dose-dependent reductions of circulating CD16/56-positive natural-killer cells with a maximum decrease occurring 8–10 weeks after initiation of therapy. The drug is metabolized 70% by the liver and 30% by the kidney. Hepatic clearance of tofacitinib is mediated predominantly by the CYP3A4 system. Therefore, a significant interaction may occur with other drugs that inhibit CYP3A4, such as ketoconazole and fluconazole, and the dose should be reduced from recommended dosing 5 mg twice daily to once daily in patients taking these drugs. A dose reduction to 5 mg daily is also recommended for patients with moderate renal or hepatic dysfunction.