In ancient Roman mythology, the two-faced Roman God Janus presided over all beginnings and transitions. On November 6, 2012, the U.S. Food and Drug Administration (FDA) approval of the first Janus kinase (JAK) inhibitor, tofacitinib, for treatment of rheumatoid arthritis (RA) heralded the advent of kinase inhibitors in the therapeutics of rheumatic diseases. Despite the advances in treatment of RA over the last two decades by the use of cytokine and target cell inhibitors, a significant percentage of RA patients either do not respond or lose their response to therapy. The pathophysiology of rheumatoid arthritis is dependent on the activation of both the innate and adaptive immune systems. The cells that comprise the immune system utilize kinases as the gatekeepers to determine how they should respond to external stimuli such as antigens, cytokines, and immune complexes. The use of new small molecule inhibitors against cytoplasmic kinases such as the JAK family, splenic tyrosine kinase (SYK), or mitogen-activated phosphokinase p38 (p38MAPK) will alter the resulting dysregulated immune systems in different ways and hopefully further promote our understanding of its complexities.
Small Molecule Mechanism of Action
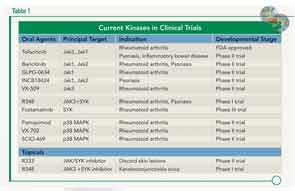
In addition to the newly released tofacitinib, at least three other JAK inhibitors are currently in phase II studies for treatment of RA, psoriasis, and inflammatory bowel disease (see Table 1). The mechanism of action of these agents is unique compared to currently available therapeutic modalities by its effect on the intracellular signaling apparatus comprising the JAK family network used by inflammatory cytokines and other growth factors. Following binding of cytokines or growth factors to their respective receptor, JAKs phosphorylate and activate members of the signal transducer and activator of gene transcription (STAT) family. Inflammatory cytokines such as interleukin (IL) 6, IL-2, and IL-12/IL-23 are dependent on the Janus family of kinases. The JAK family is composed of four tyrosine kinases. JAK-1, JAK-2, and TYK2 are expressed ubiquitously, but JAK 3 is limited to lymphoid tissues.1 All JAKs possess two similar phosphate-transferring domains, one with actual kinase activity and the pseudokinase domain, which negatively regulates the kinase activity of the first.2 This dual regulatory function led to the origin of its name, JAK, taken from the mythological god Janus represented by two faces and often present over doorways symbolizing transitions. The JAK-STAT interaction is responsible for the signal transduction of over 50 members of the 4-helix bundle cytokine family, including interferons and growth factors such as leptin, prolactin, GM-CSF, and erythropoietin (EPO).
Future studies of additional kinases will help elicit a better understanding of the complex coding mechanisms of regulation of both innate and adaptive immune systems.
Spotlight on Tofacitinib
Tofacitinib was approved for use in patients with moderate to severe rheumatoid arthritis who have had an inadequate response or intolerance to methotrexate (MTX) as monotherapy or with other nonbiological disease-modifying antirheumatic drugs (DMARDs).3 Its principal target is JAK1/JAK3. The treatment results in dose-dependent reductions of circulating CD16/56-positive natural-killer cells with a maximum decrease occurring 8–10 weeks after initiation of therapy. The drug is metabolized 70% by the liver and 30% by the kidney. Hepatic clearance of tofacitinib is mediated predominantly by the CYP3A4 system. Therefore, a significant interaction may occur with other drugs that inhibit CYP3A4, such as ketoconazole and fluconazole, and the dose should be reduced from recommended dosing 5 mg twice daily to once daily in patients taking these drugs. A dose reduction to 5 mg daily is also recommended for patients with moderate renal or hepatic dysfunction.
At the November 2012 ACR/ARHP Annual Meeting, the ORAL phase III studies for RA as well as long-term extensions were summarized in terms of efficacy and safety for both 5-mg and 10-mg p.o. b.i.d. dose schedules.4 The FDA only approved the 5-mg p.o. b.i.d. dose. Pooling data from approximately 3,300 RA patients comprising five different ORAL studies on tofacitinib treatment in RA, an ACR 20/50/70 response of 74.6%, 49.3%, and 32.8%, respectively, was observed, with 17.9% of these achieving a Disease Activity Score–defined remission. Within this population, 53.1% of patients failing two prior tumor necrosis factor (TNF) inhibitors achieved an ACR 20 response.5
The 12-month data from the ORAL START phase III trial were presented, evaluating a cohort of 958 MTX-naive patients receiving tofacitinib as monotherapy or MTX titration. Initial 12-month data are intriguing, as they demonstrated significant improvement in symptoms, physical function, and retarded radiographic progression compared to the MTX arm.6 Longer studies will be needed to see if this trend is maintained with similar safety as MTX.
Safety analyses of pooled data of tofacitinib-treated patients show a similar serious infection rate to biologics of 2.7/100 patient-years with opportunistic infections including tuberculosis, fungal infections, and pneumocystis reported. Screening for latent tuberculosis is recommended. The frequency of serious infections was increased in patients over the age of 65. In long-term extensions, a slightly higher rate of infections and nonmelanoma skin cancers was seen in the 10-mg p.o. b.i.d. studies, and this dose was therefore not approved by the FDA. However, a higher incidence ratio (4.5) of herpes zoster was seen compared to other biologics (1.32).7 There was no association with neutropenia, lymphopenia, or concomitant nonbiologic DMARDs. No safety data are available on impact of tofacitinib on patients with chronic viral hepatitis reactivation, as these patients were excluded from the trials. Prophylactic vaccination for herpes zoster and hepatitis B should be updated prior to treatment whenever possible, and live virus vaccination during treatment should be avoided.
Malignancies including lymphoma have been reported in conjunction with treatment with tofacitinib, and Epstein-Barr virus lymphoproliferative disorders were seen in renal transplant studies.
GI perforations occurred in 10 of 5,043 tofacitinib-treated patients in analysis of pooled study data from ORAL trials with long-term extensions resulting in 0.144 events per 100 patient-years. Six of these cases were diverticular in nature, three were appendiceal perforations, and one an isolated gastric ulcer.
Laboratory-test monitoring should include initially a complete blood count (CBC), comprehensive metabolic panel (CMP), and fasting lipid panel. Minor decreases in absolute lymphocyte, neutrophil, and red blood cell counts were seen in less than 1% of patients. Transaminitis was also reported, which usually responded to a reduction in dose or discontinuation of therapy with only 0.5% reaching three times the upper limit of normal on the 5-mg p.o. b.i.d. A dose-response change in creatinine (mean <0.1 mg/dl) was seen, which generally peaked at six weeks and then plateaued with a return to baseline four to six weeks after discontinuation. However, in long-term extensions, discontinuation of therapy only occurred due to renal insufficiency in 0.4% of patients in the 5-mg b.i.d. studies. The cause of this change is not understood. Mean LDL cholesterol increased by 15% and mean HDL increase by 10% with no change in LDL/HDL ratio. This effect was generally present within six weeks. A repeat fasting lipid panel is recommended at two to three months of therapy. Initial monitoring of CBC and CMP monthly for the first three months and then every two to three months thereafter would be prudent as this agent is used in larger, more heterogeneous patient populations.
Other Kinases
Splenic tyrosine kinase (Syk) is a cytoplasmic tyrosine kinase expressed predominately in hematopoietic tissues including osteoclasts that associates directly with surface receptors, including B cell receptors, Fcgamma receptors on macrophages, mast cells, and neutrophils. A SYK inhibitor, fostamatinib, has completed phase II studies demonstrating significant ACR 20/50/70 responses at doses of 100–150-mg b.i.d., better than placebo in the setting of background MTX.8 Results from its phase III studies (OSKIRA) were announced on June 4, and based on the findings, AstraZeneca has decided not to proceed with regulatory filings for fostamatinib. The studies looked at the effect of fostamatinib on RA patients with inadequate responses to DMARDs including MTX, as well as patients who fail a single anti-TNF therapy. Side effects of abnormal liver function tests, diarrhea, and neutropenia were seen, but in contrast to JAK inhibitors, an unexplained increase in blood pressure occurred. SYK inhibition may have benefit in systemic lupus erythematosus since it has the flexibility to affect B-cell receptor activation.
Other JAK/SYK inhibitor compounds for topical use are currently under investigation for treatment of active discoid lupus as well as ophthalmic preparations for keratoconjunctivitis sicca.
Unfortunately, clinical trials looking at inhibitors of p38MAPK have been disappointing. This serine-threonine kinase upon activation leads to production of TNF-α, IL-1, and IL-6 by monocytes. Despite its initial promise, phase II trials of pamapimod, VX-702+MTX demonstrated no benefit over the placebo arm despite improvement in CRP levels.9 Future studies of additional kinases will help elicit a better understanding of the complex coding mechanisms of regulation of both innate and adaptive immune systems. Hopefully, this will translate to greater selectivity of these agents, fine tuning their effect and minimizing adverse events.
The two-faced nature of the mythological god contrasts our future with our past experiences with other pharmaceutical agents. Further use in heterogeneous populations of RA with close scrutiny of safety will aid the clinician to determine the proper placement of these new small-molecule therapies in the treatment of RA.
Dr. Parks is medical director of rheumatology clinics and professor of medicine at Washington University School of Medicine in St. Louis.
References
- Laurence A, Pesu M, Silvennoinen O, O’Shea J. JAK kinases in health and disease: An update. Open Rheumatol J. 2012;6:232-244.
- Seavey MM, Dobrzanski P. The many faces of Janus kinase. Biochem Pharmacol. 2012;83:1136-1145.
- Fleischmann R, Kremer J, Cush J, et al. Placebo-controlled trial of tofacitinib monotherapy in rheumatoid arthritis. N Engl J Med. 2012;367:495-507.
- Cohen S, Krishnaswami S, Benda B, et al. Tofacitinib, an oral Janus kinase inhibitor: Analyses of efficacy and safety of 10 versus 5 mg twice daily in a pooled phase 3 and long-term extension rheumatoid arthritis population [Abstract 2485]. Arthritis Rheum. 2102;64 (Suppl.):S1048.
- Burmester GR, Blanco R, Charles-Schoeman C. Short and long term efficacy of tofacitinib, an oral Janus kinase inhibitor, in the treatment of patients with RA and an inadequate response to TNF inhibitors: Analyses of pooled phase 2, phase 3, and long term extension studies [Abstract L12]. Arthritis Rheum. 2102;64:4172.
- Lee EB, Fleischmann RM, Hall S, et al. Radiographic, clinical and functional comparison of tofacitinib monotherapy versus methotrexate in methotrexate-naive patients with rheumatoid arthritis. [Abstract 2486]. Arthritis Rheum. 2102;64 (Suppl.):S1049.
- Winthrop KL, Valdez H, Mortensen E, et al. Herpes zoster and tofacitinib therapy in patients with rheumatoid arthritis [Abstract 2490]. Arthritis Rheum. 2102;64 (Suppl.):S1051.
- Morales-Torres J. The status of fostamatinib in the treatment of rheumatoid arthritis. Expert Rev Clin Immunol. 2012;8:609-615.
- Kyttaris VC. Kinase inhibitors: A new class of antirheumatic drugs. Drug Des Devel Ther. 2012;6:245-250.