A genetically engineered T cell.
SAN DIEGO—At the 2017 ACR/ARHP Annual Meeting this past November, an expert said researchers are making progress in identifying drugs that can correct problems with transcriptional programming, which, if perfected, could go a long way toward harnessing more fully the power of genetics knowledge and directing it toward patient care. The session also delved into how researchers are working to apply a strategy similar to chimeric antigen receptor (CAR) T cell therapy to autoimmune disorders.
Controlling Transcription
Most of the genetic variants identified in genome-wide association studies (GWAS) map to noncoding DNA, and there’s a growing understanding that the vast majority of this noncoding DNA involves gene enhancers and repressors that can regulate transcriptional programs, said Dennis Carson, MD, professor of medicine at the University of California, San Diego.
“We do not yet have methods to identify drugs that can modify and, hopefully, correct aberrant transcriptional programs,” he said. “This is what we’re taking a stab at in our lab.”
Dr. Carson has pursued this line of research for a decade. The challenge, in part, is that what’s encoded are not proteins, and the enhancer or repressor effect depends on the cellular context, so organism-wide targeting could produce undesirable effects. Plus, multiple enhancers and repressors work together in complex ways to control the transcriptional programs.
Dr. Carson’s center has approached the problem with a high-throughput process to examine how drugs or compounds regulate the transcriptional response when a stimulus is applied.
“Our idea was you might be able to find improved approaches for the discovery of immune regulatory drugs by looking at drugs or compounds that regulate the magnitude of transcriptional response to a stimulus, the kinetics of a transcriptional response and breadth of a transcriptional response,” he said.
Using biochemical and computational methods, the researchers look for compounds that act either as an immune enhancer and slow the response to the stimulus, or as an immune repressor and speed it up—all without affecting the basic physiology of the response. They’ve looked at the NF-kappa-beta and interferon pathways.1
To pare down the compounds to legitimate contenders, the researchers first focused on those that feature kinetics similar to other compounds and might hit the same target, and that have similar chemical structures to others, making it much more statistically likely they’re true hits. Then researchers moved to RNA sequencing to further validate the compounds.
So far, they’ve found immune enhancers that potentiated Type 1 T helper cells in vivo when co-administered with a TLR4 agonist, as well as repressors that were orally bioavailable and suppressed experimental arthritis in two animal models.
“If we’re going to do anything about all these noncoding regions that influence cancer and immunity and inflammation, [we] need improved cell-based assays that faithfully mimic disease-associated transcriptional programs,” said Dr. Carson, mentioning potentially using patient-derived monocytic and lymphocytic cell lines, or CRISPR gene editing. “We have the technology to do it.”
CAR T Cell Therapy, Reversed?
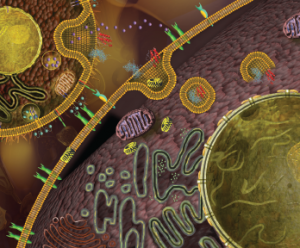
Michael Milone, MD, associate professor of pathology and laboratory medicine at the University of Pennsylvania in Philadelphia, showed how the strategy of CAR T cell therapy might be tweaked to treat autoimmune disorders.
In CAR therapy, developed for hematologic malignancies and now the subject of 123 trials around the world, T cells are drawn from patients, reengineered to express receptors for a targeted antigen, and readministered, where they propagate and have produced stunning, durable responses in lymphoma and other blood cancers.
“Could we reverse this CAR system, so we present the antigen instead of the antibody on the surface of the CAR, allowing us to get antigen-specific B cell targeting?” Dr. Milone asked.
Work at his center has focused on pemphigus vulgaris (PV), in which antibodies form against molecules called desmogleins that help form the adhesive junction between epithelial cells. With no FDA-approved therapies for the disease, treatment typically has involved mycophenolate, azathioprine or methotrexate. Rituximab has yielded good results, but the responses haven’t proved durable.
Capitalizing on knowledge of the structure of the pathogenic desmoglein antibodies involved in PV, researchers designed a chimeric autoantibody receptor (CAAR) to target specific desmoglein domains. In mouse models, this approach has eliminated desmoglein 3-specific B cells.2
Dr. Milone said the approach (and cell therapy in general) holds a lot of promise and could open a new avenue of therapies for rheumatologists.
“T cells are a very viable therapeutic platform,” he said. “We’ve only begun to scratch the surface on the types of cells we can engineer.”
Thomas R. Collins is a freelance writer living in South Florida.
References
- Chan M, Ahmadi A, Yao S, et al. Identification of biologically active pyrimido[5,4-b]indoles that prolong NF-κB activation without intrinsic activity. ACS Comb Sci. 2017 Aug 14;19(8):533–543.
- Ellebrecht CT, Bhoj VG, Nace A, et al. Reengineering chimeric antigen receptor T cells for targeted therapy of autoimmune disease. Science. 2016 Jul 8;353(6295):179–184.