Since clinical trials generally focus on several primary endpoints (e.g., relief of signs and symptoms of disease, improvement in patient-reported outcomes, and inhibition of structural progression of disease), it would seem that an objective metric that is a composite outcome measure makes the most sense. As rheumatologists, however, we feel strongly that any composite measure needs to include an assessment of tender and swollen joints, since these are the principal “target organ” of rheumatoid arthritis. One thing seems clear from the available data, however: in the absence of an objective metric and a specific goal or target, it can be difficult to justify alteration in therapy, whether dose escalation of one medication, such as methotrexate, or addition of another, such as a biologic agent.
Given the importance of a target, we must first recognize our goal in treating RA to target. Is our goal to reduce pain in the present? To reduce disability in the future? To reduce associated cardiovascular mortality? All of the above?
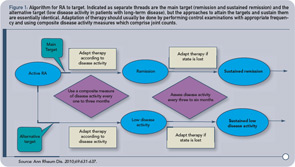
Next, we must determine the frequency with which we evaluate patients for their achievement of target. Should we be monitoring patients every month? Every three months? We feel that the frequency of evaluation should ultimately depend upon the patient’s level of disease activity, with patients with higher disease activity requiring more frequent monitoring.
Finally, we must take into consideration the rate at which different patients achieve their targets, and decide how important is the speed with which they achieve their targets. Is reaching the target over a three-month period better than reaching it over a six- to nine-month period? Do we initiate therapy with a DMARD and then escalate with a second DMARD or biologic as needed, or do we initiate therapy with multiple agents at once and then reduce the dose of one or more agent as the disease comes under control?
Of course, patients must be partners in the decision to treat to target. The escalation of therapy with a biologic, for example, requires willingness on the patient’s behalf either to self-inject medication or to schedule an appointment at an infusion center for intravenous administration. Patients must also monitor themselves closely for any signs of infection, as the presence of infection is a limiting factor to the escalation of therapy.
