ellepigrafica / shutterstock.com
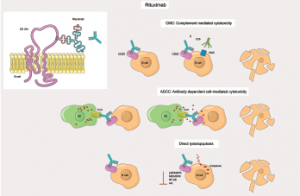
Severe infections occurred in 25% of patients with anti-neutrophil cytoplasm antibody (ANCA) associated vasculitis (AAV) who were treated with rituximab, according to results of an observational study conducted in the United Kingdom (U.K.) and Austria. Trimethoprim-sulfamethoxazole (TMP/SMX) prophylaxis, however, reduced the risk of severe infections, the investigators reported in Annals of the Rheumatic Diseases.1
Andreas Kronbichler, MD, PhD, at the Vasculitis and Lupus Clinic, Addenbrooke’s Hospital, Cambridge, U.K., says the risk of severe infections with rituximab therapy “is sevenfold higher than in rheumatoid arthritis in patients with ANCA-associated vasculitis. Antibiotic prophylaxis with TMP/SMX helps reduce the risk by 70%, at least in our investigation.”
Patients with preexisting or ongoing lung damage or involvement are at “particular risk to develop severe infections,” Dr. Kronbichler says.
The aim of the study was to assess the frequency of severe, life-threatening infection and identify the risk factors for development of severe infection, classified as [Common Terminology Criteria for Adverse Events] CTCAE grade ≥3, in patients with AAV who received rituximab. One hundred ninety-two patients with AAV who had been referred for rituximab to two tertiary care specialist centers in Cambridge and Innsbruck, Austria, between 2004 and 2014 were included in the study. Among the 192 patients, 134 were diagnosed with granulomatosis with polyangiitis (GPA), 28 with microscopic polyangiitis (MPA), and 30 with eosinophilic granulomatosis with polyangiitis (EGPA).
“The risk of severe infections was higher than I expected before starting collection of data,” Dr. Kronbichler says.
Follow-up, which began when rituximab therapy was initiated, ended two years later or when a patient died or was lost to follow-up. Mean follow-up was 22.67 months. The researchers found that respiratory tract infections were the leading cause of severe infections. Additionally, they found an association of endobronchial involvement, bronchiectasis and rituximab use for major relapses with severe respiratory tract infections.
Risk Factors for Severe Infection
Forty-nine patients experienced a total of 95 severe infections, according to the study, an event rate of 26.06 per 100 person-years. Although respiratory tract infections (n=63) were the most common infectious complications among this population, other types included urinary tract (n=12), gastrointestinal tract (n=8), mastoiditis/otitis externa (n=4), skin (n=3), sepsis/septicaemia with unidentified site of infection (n=1) and others.
Twenty-five percent of observed infections occurred in the first four months of follow-up, 50% after 12 months and 80% after 18 months.
For those cases with a positive microbial result, opportunistic pathogens identified included Pseudomonas aeruginosa (n=4), Staphylococcus aureas including methicillin-resistant strains (n=4), Escherichia coli (n=3), Clostridium difficile (n=2), Pneumocystis jirovecii (n=1), Legionella pneumophila (n=1) and invasive aspergillosis (n=1). Campylobacter jejuni gastroenteritis was observed in one case.