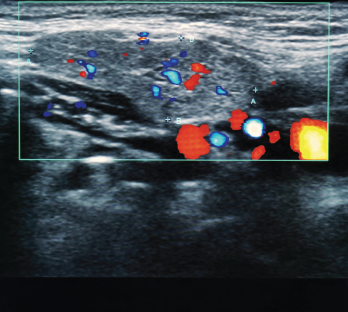
An ultrasound image of the submandibular salivary gland.
Flowersandtraveling / shutterstock.com
For most rheumatologists, the key elements of the physical exam—inspection, palpation, percussion and auscultation—have long been second nature, but a fifth modality has grown in importance with respect to making the correct diagnosis: ultrasound.
From evaluating for Doppler signal and additional findings indicative of synovitis to identifying bony erosions, chondrocalcinosis, tophi and other articular and periarticular pathology, ultrasonography has become more and more valuable as a clinical tool for practicing rheumatologists.
Amy Evangelisto, MD, past president of the Ultrasound School of North American Rheumatologists (USSONAR) and current clinician with Arthritis, Rheumatic & Back Disease Associates, New Jersey, was among the first U.S. rheumatologists to seek additional training in rheumatologic musculoskeletal ultrasound in Leeds, England, in the early 2000s.
“When I became interested in musculoskeletal ultrasound,” says Dr. Evangelisto, “there were no rheumatology-focused courses or training programs in the U.S., so we had to rely on radiology-based courses or find other pathways on our own. Now we are lucky to have so many excellent resources available for rheumatologists interested in learning ultrasound.”
Today, Dr. Evangelisto regularly uses ultrasound in her clinical practice, both to aid diagnosis and for guided injections. She is also active in USSONAR efforts to increase the knowledge of and competency in ultrasound across the field of medicine.
Training
Training in ultrasound has, in recent years, spread much more diffusely across the medical education landscape. In a survey of 82 U.S. MD-granting medical schools, 62% of curricular administrators responded that ultrasound training is incorporated into their medical school’s curriculum, with 46% noting that the training is part of the student’s third year (i.e., at the start of their clinical training).1
Similarly, in a survey of 108 rheumatology fellowship training program directors, 94% responded their program teaches musculoskeletal ultrasound and 41% have a formal ultrasound curriculum. Close to 80% of programs teach image optimization, normal anatomy, disease-specific pathology and ultrasound-guided procedures, 51% cover ultrasound physics, and 43% discuss documentation and billing for ultrasound.2
With respect to internal medicine residency training, the Alliance for Academic Internal Medicine (AAIM) issued a position statement in 2019 recognizing and supporting the integration of point-of-care ultrasound (POCUS) across undergraduate, graduate and continuing medical education, but several barriers have been identified, including lack of POCUS-trained faculty and/or ultrasound equipment, and lack of crucial image archival systems and quality assurance.3
Karina Torralba, MD, division head and fellowship program director in the Division of Rheumatology at Loma Linda University School of Medicine, Calif., notes that some additional challenges to incorporating ultrasound teaching into curricula are the limited time allotted to this purpose and restrictions on a provider’s ability to bill for these services.
Dr. Torralba explains that, from an educational perspective, the question is: When will issues other than those that are purely musculoskeletal be included in ultrasonography teaching and evaluation? For example, salivary gland ultrasonography is now recognized as a potentially valuable and specific tool for the early recognition of Sjögren’s syndrome.4
Similarly, color duplex sonography of the temporal arteries has shown promise in helping diagnose giant cell arteritis, with edema throughout the wall of the vessel and resulting periluminal hypoechoic halo (referred to as the halo sign) showing higher sensitivity than arterial biopsy and bilateral halo sign reaching a specificity of nearly 100%.5
As more anatomic locations and clinical conditions can be explored with ultrasonography, the potential value of this tool increases and the ways in which it can and should be incorporated into rheumatologic training multiply.
Novel Uses
Novel uses of ultrasound are currently being explored, including the best way to make use of all data captured from this instrument. Myma Albayda, MD, director of the Musculoskeletal Ultrasound and Injection Clinic and assistant professor of medicine in the Division of Rheumatology at Johns Hopkins University School of Medicine, Baltimore, has been studying the use of ultrasound for muscle evaluation in myositis.
In collaborating with engineers at the Applied Physics Lab at Johns Hopkins, she has used machine learning and deep learning techniques for image analysis. In a study of 80 subjects with myositis, more than 3,000 ultrasound images of seven muscles (observed bilaterally) were acquired. The authors used traditional machine learning techniques, as well as an automated deep learning method that employed deep convolutional neural networks (DL-DCNNs), to consider three problems of classification, including normal vs. any form of myositis, normal vs. inclusion-body myositis (IBM), and IBM vs. other types of myositis. They found that DL-DCNN-based classification improved the accuracy of all classification problems, while providing a fully automated approach to classification.6
The authors surmise that data-driven approaches picked up by deep learning assessment the entire image are superior to manually selected features. Dr. Albayda notes, “As the first application of artificial intelligence techniques to muscle ultrasound, this is promising for enhancing accuracy, efficiency and decreasing subjectivity with ultrasound studies.”
The ACR Position
In this context, it is no wonder the ACR published a position statement in 2018 noting that musculoskeletal ultrasound is a useful tool for the diagnosis, management and treatment of rheumatic conditions and that the ACR encourages rheumatologists to pursue “suitable training and a certification process of their choice.”7
With additional research and education in the field, it seems clear that ultrasound is a useful tool for rheumatologists now and will remain so for many years to come.
Jason Liebowitz, MD, completed his fellowship in rheumatology at Johns Hopkins University, Baltimore, where he also earned his medical degree. He is currently in practice with Skylands Medical Group, N.J.
References
- Bahner DP, Goldman E, Way D, et al. The state of ultrasound education in U.S. medical schools: Results of a national survey. Acad Med. 2014 Dec;89(12):1681–1686.
- Torralba KD, Cannella AC, Kissin EY, et al. Musculoskeletal ultrasound instruction in adult rheumatology fellowship programs. Arthritis Care Res (Hoboken). 2020 Jun;72(6):859–870.
- LoPresti CM, Jensen TP, Dversdal RK, Astiz DJ. Point-of-care ultrasound for internal medicine residency training: A position statement from the Alliance of Academic Internal Medicine. Am J Med. 2019 Nov;132(11):1356–1360.
- Baldini C, Luciano N, Tarantini G, et al. Salivary gland ultrasonography: A highly specific tool for the early diagnosis of primary Sjögren’s syndrome. Arthritis Res Ther. 2015 May 28;17(1):146.
- Monti S, Floris A, Ponte C, et al. The use of ultrasound to assess giant cell arteritis: Review of the current evidence and practical guide for the rheumatologist. Rheumatology (Oxford). 2018 Feb 1;57(2):227–235.
- Burlina P, Billings S, Joshi N, Albayda J. Automated diagnosis of myositis from muscle ultrasound: Exploring the use of machine learning and deep learning methods. PLoS One. 2017 Aug 30;12(8):e0184059.
- American College of Rheumatology Committee on Rheumatologic Care. Position statement: Musculoskeletal ultrasound. 2014 Feb; updated 2018 Aug.
Learn More
The ACR recognizes the importance of demonstrating knowledge and competency for performing musculoskeletal ultrasound, and has created a rheumatology-specific training and certification program.



