Ankle
Half of the participants stumbled in visualizing the posterior tibial tendon (PTT) insertion. The course of the PTT in the ankle and foot is as follows: around the posterior portion of the medial malleolus, then on the cranial surface of the sustentaculum tali, then inferior to the calcaneo-
navicular (i.e., spring) ligament. Finally, as it gets to the navicular, about half of its fibers attach to the navicular tuberosity (infero-medial surface of the navicular) and the medial cuneiform. Some recurrent fibers connect to the sustentaculum tali, and the remaining fibers continue to the plantar surface of the foot. Due to this unusual course, when imaging the PTT in its longitudinal view in the medial foot, the sound beam must be angled slightly cephalad to minimize anisotropy.4
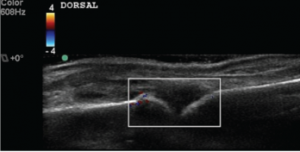
A few fellows misidentified calcaneal erosion as osteophytes due to failure to correlate longitudinal with transverse images and construct a three-dimensional image of the Achilles insertion in their minds. Erosions are potholes in the bone, and osteophytes are jagged extrusions from the bone. These two will be confused only if the sonographer cannot determine where the normal bone surface is, and this mistake could lead to substantial diagnostic and treatment errors (see Figure 1). At this moment, the student tends to feel like a heel (sic, you know who).
1st Metatarsalphalangeal Joint
The synovial reflection for the dorsal aspect of this joint is superficial and easily compressed by even light transducer pressure. Many students scan the first MTP without floating the transducer, a technique in which a thick layer of gel is maintained between the surface of the skin and the transducer face to minimize tissue pressure. The small effusion the model had was missed by the students who did not employ the floating technique.
The other difficulty for students included obtaining a longitudinal view of the plantar/volar metatarsal head due to shadowing from the sesamoid bones, and some resulting confusion of the sesamoid bones with the metatarsal head. The metatarsal head is deeper and has a layer of hyaline cartilage that the sesamoids do not. Often, the transducer frequency must be lowered for this view to penetrate the thick plantar soft tissues.
The Bottom Line
Despite a formal standardized training program, considerable variability in participant performance on written and practical examinations exists. We believe our final exam results not only evaluate competence, but also help fill in skill and knowledge gaps among the trainees and align their confidence to their competence. The ACR’s Musculoskeletal Ultrasound Certification in Rheumatology (RhMSUS) certification examination in musculoskeletal ultrasound also serves this important purpose: to let the practitioner know whether their ultrasound knowledge level meets acceptable standards. This is a very valuable service to the rheumatology community and our patients.
Although RhMSUS does not include a practical examination, there is a very high correlation between the participant scores on the written and practical portions of other examinations.5