 When Beverly Johnson, MD, became the chief of rheumatology at Jacobi Medical Center & North Central Bronx Hospital in New York more than two years ago, she was already trained in musculoskeletal ultrasound.
When Beverly Johnson, MD, became the chief of rheumatology at Jacobi Medical Center & North Central Bronx Hospital in New York more than two years ago, she was already trained in musculoskeletal ultrasound.
Unfortunately, as a safety net hospital that treats a lot of undocumented and uninsured patients, the hospital didn’t have the budget for an ultrasound machine. But the hospital’s auxiliary program was able to purchase one. “We wanted to give the best possible care to patients, regardless of their income status,” says Dr. Johnson.
Dr. Johnson began using the ultrasound machine on her patients. “The fellows became interested in learning this technology, and patients expressed interest in getting ultrasound-guided injections and diagnostic ultrasounds,” she says.
Given this, Dr. Johnson, who is also an assistant professor of medicine at Albert Einstein College of Medicine, started a series of lectures for the rheumatology fellows on how to perform ultrasounds and began taking the machine on inpatient rounds and clinics. “Because of its popularity, we decided to create a separate clinic just for ultrasound,” she says.
To do this, Dr. Johnson had to negotiate space to run the clinic, get referring physicians on board to recommend the clinic and instruct administrative personnel on how to bill for it.
What It Can Do
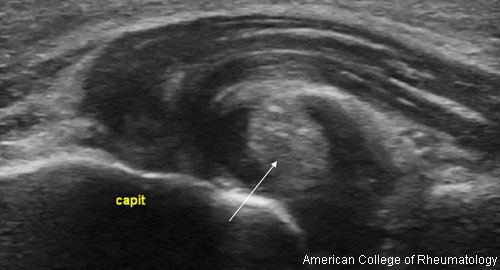
Rheumatologists both administer ultrasound and interpret the findings. When it comes to rheumatology patients, an ultrasound machine has a lot of uses. It can diagnose problems, such as rotator cuff tears and bone erosions that can occur with rheumatoid arthritis (RA), as well as show active inflammation in patients with gout and RA. “It can also help diagnose patients when there is no clear-cut diagnosis,” Dr. Johnson says.
In addition, ultrasound gives rheumatologists a more accurate way to inject a joint. Instead of using an anatomical landmark, they have a visual of the needle entering the joint.
Studies have shown that the accuracy of joint injections improves significantly when employing ultrasound.1,2 “This is ultimately better for patient care,” Dr. Johnson says. In fact, the results of a patient satisfaction study done at Jacobi regarding ultrasound-guided vs. landmark-guided injections was presented at the 2016 ACR/ARHP Annual Meeting as a poster session. (For more information, see Imaging of Rheumatic Diseases—Poster Session I: Ultrasound and Emerging Technologies.)
From a diagnostic point of view, Dr. Johnson finds ultrasound to be quite cost effective. Low-income patients in the hospital’s fee-scaled program can have ultrasound performed while they are at the clinic at no extra charge. Without the ultrasound machine, patients would need to have magnetic resonance imaging—which would cost much more to perform. In the past year, more than 100 patients at Jacobi Medical Center & North Central Bronx Hospital have been treated with ultrasound.



