Image Credit: Nicotombo/shutterstock.com
Two months into the transition, the ICD-10 code set is still not exactly the most enticing reading material. But there is still so much to learn and apply, that it is necessary for physicians, coders and billers to stay abreast of the coding and billing guidelines. Although all of the guidelines and conventions may be overwhelming, it’s imperative to understand the level of coding that is necessary to avoid denials or rejections. One main focus of ICD-10 in the media and practices nationwide is that of external cause codes, but a specific focus for rheumatology practices is understanding the difference between using external cause codes and status codes.
We constantly hear of “freak accidents” and wonder sometimes if the reports are even real. But a lot of this comes into reality when looking through the ICD-10 manual and seeing such codes as W61.02xA, struck by parrot, initial encounter, or W55.32xA, struck by other hoof stock, initial encounter. External cause codes are intended to provide data for injury research and evaluation of injury-prevention strategies. These codes capture how the injury or health condition happened; the intent, whether unintentional or accidental, or intentional, such as suicide or assault; the place where the event occurred or the activity of the patient at the time of the event; as well as the person’s status (e.g., civilian, military).
The Centers for Medicare & Medicaid Services states that, “There is no national requirement for mandatory ICD-10-CM external cause code reporting. Unless a provider is subject to a state-based external cause code reporting mandate or these codes are required by a particular payer, reporting of ICD-10-CM codes in Chapter 20, External Causes of Morbidity, is not required. In the absence of a mandatory reporting requirement, providers are encouraged to voluntarily report external cause codes, as they provide valuable data for injury research and evaluation of injury prevention strategies.”
Keep in mind that some states require tracking of different diagnoses and procedures for public health reasons. So there may be some less absurd ICD-10 codes required by law, and this will need to be monitored by individual states.
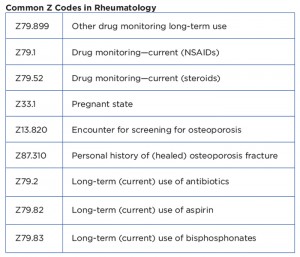
On the other hand, a Z code (replacing the V codes in ICD-9) represents reasons for some encounters and requires a corresponding procedure code to accompany the Z code if a procedure is performed. They are a special group of codes provided in ICD-10-CM for the reporting of factors influencing health status and contact with health services. Z codes are designated as the principal/first listed diagnosis in specific situations such as:
- To indicate that a person with a resolving disease, injury or chronic condition is being seen for specific aftercare, such as the removal of internal fixation devices, such as orthopedic pins;
- To indicate that a person is seen for the sole purpose of special therapy, such as chemotherapy, immunotherapy and radiation therapy; or
- To indicate that a person not currently ill is encountering the health service for a specific reason.
The significant change between the two coding classifications is that ICD-9-CM’s supplementary codes are now incorporated into the main classification in ICD-10-CM. This integration has allowed Z codes to gain recognition with their own chapter in the manual and can be found in Chapter 21, Factors Influencing Health Status and Contact with Health Services. The increased specificity of Z codes is designed to help with understanding why the patient was seen for the date of service and will eventually help get claims paid faster and with fewer errors, and minimize requests for medical records or chart reviews, as they will clearly guide the reason for the visit. The similarities of the coding categories are the general intent to report issues, other than diagnoses, regarding health status or contact with health services for a patient.
It’s important to understand that status codes are informative; they have distinct categories for certain encounters and conditions. They can be reported in any health setting and may be used as a first-listed diagnosis (depending on the encounter or if for an inpatient setting) or secondary code, depending on the circumstances for the encounter. Status codes indicate that a patient is a carrier of a disease, has the sequelae or residual of a past disease or condition, or has another factor influencing their health status. Because status codes may affect the course of treatment and its outcome, the codes are used to track public health issues.
Are Z codes mandatory? The Official Coding Guidelines do not differentiate the use of Z codes from that of other codes (except W external codes). Z codes will most often be used to describe an encounter for testing or to identify a potential risk. In the case of using it as a principal diagnosis, this can be used mainly for osteoporosis. If there are no signs or symptoms of osteoporosis documented in a patient’s record, the screening code is correct. Although there are no specific coding rules for ICD-10 on this issue, the coding guidelines for ICD-10 are the same as ICD-9 (use screening: if there are no signs/symptoms, then the screening code should be used, but if there are signs/symptoms, then a specific diagnosis code should be applied). For example, if a postmenopausal patient undergoes a bone density study for screening for osteoporosis, Z13.820 (encounter for screening for osteoporosis) is recommended as the first code, and Z78.0 (asymptomatic menopausal state) as a secondary code.
Additionally, in ICD-10, some status codes are required to accompany another main or principal diagnosis, if applicable, and are usually listed under the category in the tabular list of the code. For example, E66 (overweight and obesity) indicates use of an additional code to identify body mass index (BMI), if known (Z68.-), or M81.0 (age-related osteoporosis without current pathological fracture), personal history of (healed) osteoporosis fracture, if applicable (Z87.310).
Although a lot of questions about using the ICD-10 code sets remain, it’s important not to take things out of context, because the rules and guidelines for diagnosis coding have not changed. The official coding guidelines should be consulted for all coding and sequencing decisions made when the ICD-10-CM conventions do not provide specific directions.
For questions or additional information on coding ICD-10, contact the ACR coding and practice management team or visit the ACR website for a rheumatology-specific ICD-10 crosswalk and superbill to assist with general mapping.