Although there are seven components for the levels of evaluation and management (E/M) services, most encounter levels are coded on the basis of the history, examination and medical decision making (MDM), which are the key components extracted from documentation in the medical record. However, when counseling and coordination of care for a patient are the predominate activities in the visit, time is the component that can be used to appropriately capture the level of E/M service.
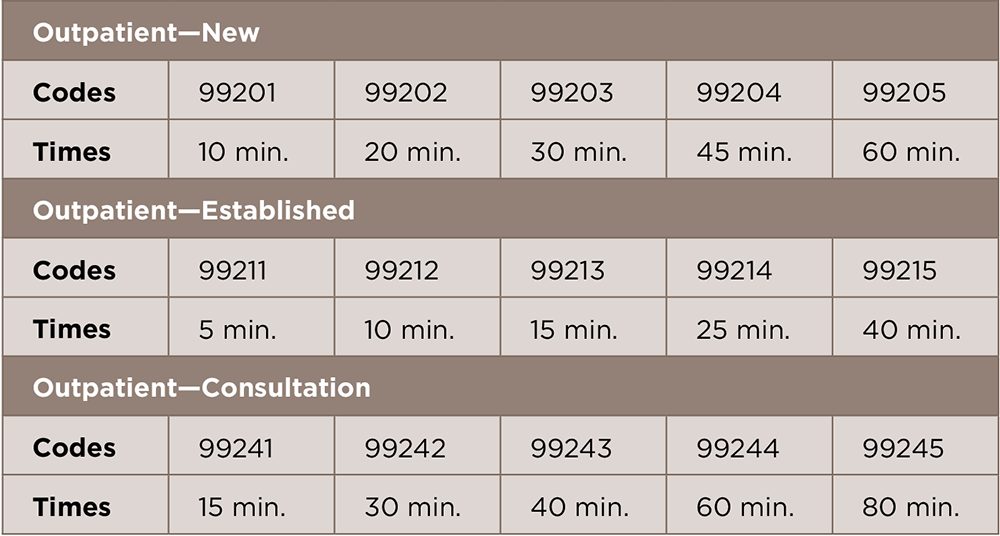
In 1992, time was included as an explicit factor for several categories of E/M services, including office visits, consultations and inpatient services. The time associated with these codes in the CPT Evaluation and Management Service guidelines is considered the average time spent providing a particular level of care to a patient (see Table 1, below, for time codes for outpatient services). To determine when to use time as the key or controlling factor, providers and their coding staff should refer to the specific details outlined in the CPT Evaluation and Management Service guidelines:
- Counseling and/or coordination of care dominates (more than 50%) the patient encounter;
- The E/M service must have a reference time identified in the code descriptor;
- Time must be spent face to face with the patient and/or family member in the office/other outpatient setting or floor/unit time in the hospital or nursing facility; and
- The extent of the counseling and/or coordination of care must be documented in the medical record.
This means that time alone can be used to select a level of care, regardless of the extent of the history, exam or MDM, if the majority of the encounter involves counseling or coordination of care. For E/M services, counseling may include a discussion of test results, diagnostic or treatment recommendations, prognosis, risks and benefits of management options, instructions, education, compliance and/or risk factor reduction.
But be careful, because it is important to remember criteria are attached to the time component as much as to the history, examination and MDM. Keep in mind when selecting a level of service on the basis of the extent of the history, examination or MDM, sufficient details must be included in the medical record to apply the most accurate level. For example, the provider cannot simply document, “I performed a comprehensive history.” Instead, the provider must document detailed information that is relevant to the patient’s history of present illness, the number of systems reviewed, and past, family and social history. Also, the MDM is not based on a single statement, but is calculated on the basis of the number and type of details documented for each component. The same rationale holds true when using time as the main factor for coding the encounter.
What really counts when coding is the basis of time. First, only face-to-face time with the patient and/or family member counts in the outpatient setting. Face-to-face time includes not only the time spent counseling, but also the time associated with any history, examination or MDM that is performed. Time spent reviewing records, talking with other providers and documenting the encounter without the patient or family present cannot be considered.
Second, it is not enough to document only how long the service lasted or that counseling or coordination of care dominated the visit. The documentation must explain the content of the counseling discussion and must describe the activities to coordinate care to support time as the dominating factor, but most importantly, the medical necessity of the service.
The Centers for Medicare & Medicaid Services (CMS) Medicare Claims Processing Manual, chapter 12, section 30.6.1.C, indicates:1 “Advise physicians that when counseling and/or coordination of care dominates (more than 50%) the face-to-face physician/patient encounter or the floor time (in the case of inpatient services), time is the key or controlling factor in selecting the level of service. In general, to bill an E/M code, the physician must complete at least two out of three criteria applicable to the type/level of service provided. However, the physician may document time spent with the patient in conjunction with the medical decision making involved and a description of the coordination of care or counseling provided. Documentation must be in sufficient detail to support the claim.”
Medicare CMS emphasizes that the CPT code selection is based on the total time of the face-to-face encounter and not just the counseling time, because counseling can also be provided by another staff member, which cannot be included in the encounter as physician–patient face-to-face time.
Quantity of information does not always equal quality, so it is not enough to simply list your clinical impressions and state that more than 50% of the encounter was spent in discussion. This is not sufficient documentation for time-based coding. If the medical record lacks the pertinent details required to justify the counseling and/or coordination of care, then this can cause unintended consequences and failure to meet the requirements to use time as the deciding factor in the E/M level.
Although it is not necessary to document a detailed account of the discussion, the documentation should reflect the nature of the counseling or coordination of care activities to identify the major areas of discussion (e.g., “counseled patient regarding weight gain, daily food intake and goalsetting”); it is important the patient record be thorough enough to justify the amount of time reported.
It is vital for providers to implement best practices in documenting time-based E/M services. Below are three important components to keep in mind to include in the patient’s medical record when using time as the key factor for a level of service:
- Document the total time of the visit;
- Include the total time spent in counseling and/or coordinating care; and
- Provide a summary of the discussion.
For questions or additional information on coding guidelines and documentation for your organization, contact the ACR coding and auditing professionals at [email protected].
Reference
- Centers for Medicare & Medicaid Services. CMS Manual System. Pub 100-04 Medicare Claims Processing. Transmittal 1875. 2009 Dec 14.