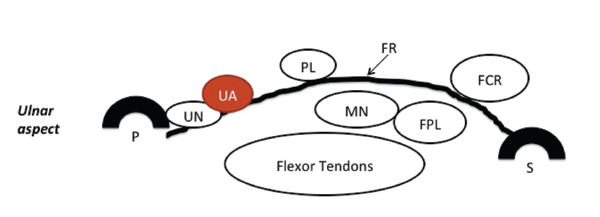
Figure 1: A schematic of normal carpal tunnel anatomy. FR = flexor retinaculum; PL = palmaris longus tendon; FCR = flexor carpi radialis tendon; FPL = flexor pollicis longus tendon; MN = median nerve; UA = ulnar artery; UN = ulnar nerve; P = pisiform bone; S = scaphoid bone. Reprinted with permission from Greenberg MH. Manual of musculoskeletal ultrasound protocols (2018).
The patient has remained asymptomatic since the injection was performed, and the anti-rheumatic medical regimen was intensified more than eight months ago.
Discussion
Carpal tunnel syndrome (CTS) results from any cause that increases pressure within the carpal tunnel, including enlargement of any of the nine flexor tendons or their coverings that pass through it (e.g., inflammation of the synovial sheaths). The median nerve is the most sensitive structure in the tunnel, supplying the first three-and-a-half digits. Compression of the median nerve may cause paresthesia, hypoesthesia, anesthesia or forearm/wrist/hand pain, and it can progress to loss of finger strength.2 The prevalence of CTS in the general population as defined by clinical evaluation and electrophysiological studies (EPS) measures 2.7%.1
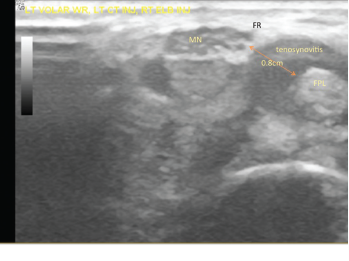
Figure 2: The patient’s left volar wrist ultrasound, transverse view (MN = median nerve; FPL = flexor pollicis longus; FR = flexor retinaculum).
Multiple risk factors may affect the median nerve separately or in concert, including occupational or other causes of excessive wrist flexion, using vibrating tools, trauma, tenosynovitis (due to rheumatoid arthritis, other connective tissue diseases, spondyloathropathy, sarcoidosis or CPPD), female gender, obesity, amyloid, hypothyroid, pregnancy, a congenitally small carpal tunnel, aberrant structures within the carpal tunnel (e.g., a ganglion cyst, a neoplasm, gouty tophus, a lipoma, accessory muscles, a bifid median nerve, a persistent median artery, osteoarthritis, an aberrant bone), diabetes, acromegaly, use of aromatase inhibitors and genetic predisposition.3
Unilateral or bilateral CTS may be a presenting symptom in rheumatoid arthritis, and it may occur anytime during the disease course, particularly with suboptimal control of synovitis. The likelihood of having CTS is increased among patients with rheumatoid arthritis.4
CTS diagnosis occurs clinically. A typical history features painful paresthesia involving some or all of the first three-and-a-half fingers, and may include decreased sensation and hand weakness. Pain may radiate retrograde into the forearm and occasionally to the shoulder. Pain is often worse at night. A physical exam may demonstrate objective hypoesthesia, hand weakness, positive Tinel’s and/or Phalen’s signs, and thenar atrophy.
Electrophysiological studies (EPS) are corroborative if abnormal.5 However, EPS may be completely normal in 10–15% of clinical CTS cases.6 To complicate matters, one study found the false positive rate to be 18%.7


