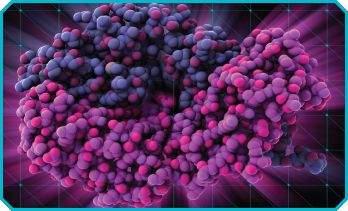
An ustekinumab molecule.
LAGUNA DESIGN/Science Source
In a multicenter, prospective, open-label study, ustekinumab therapy was effective in treating oral ulcers resistant to colchicine in patients with Behçet’s disease, according to study author David Saadoun, MD, PhD, Department of Internal Medicine and Clinical Immunology, Sorbonne University, Paris, and fellow researchers.1
Researchers focused on the topic because oral ulcers are often disabling, have an effect on quality of life and are resistant to conventional treatment.
Colchicine is typically recommended after topical measures for oral ulcers, but evidence regarding its effectiveness is lacking, according to the authors. Immunosuppressive drugs, such as azathioprine, as well as apremilast, thalidomide, interferon alpha (IFN-α) and tumor necrosis factor alpha (TNF-α) inhibitors may be used to treat oral ulcers, but these often have unwanted side effects.
Ustekinumab, which was approved in the U.S. to treat oral ulcers caused by Behçet’s disease in June 2019, is a humanized monoclonal antibody against interleukins (IL) 12 and 23.
“Interleukin-23 is critical for the differentiation of Th17 lymphocytes, and previous studies have demonstrated the critical role of Th1 and Th17 in the pathogenesis of [Behçet’s disease] and the correlation of these cytokines with disease activity,” the authors wrote.
Study Details
The current study included 30 adult patients (16 men; 14 women) who met International Study Group for Behçet’s Disease criteria and who—despite colchicine treatment—had at least one oral ulcer within 28 days before inclusion and at least two oral ulcers at the time of inclusion. The median age at the start of treatment was 39 years (range: 33–45 years old). Patients were assessed for their number of oral ulcers, joint involvement and level of disease activity. Clinical parameters, safety, daily steroid dose and lab findings were collected at the start of the study and at weeks 4 and 12, as well as every 12 weeks until treatment stopped or the end of follow-up.
Patients received 90 mg of ustekinumab subcutaneously at weeks 0 and 4 and then every 12 weeks, which is the recommendation in France for maintenance therapy for Crohn’s disease. Other therapies, such as prednisone, colchicine and other immunosuppressive therapies, were allowed if they were given at a stable dose over the month prior to inclusion and during the study period.
The study’s primary endpoint was the proportion of patients with complete response at week 12. Among the secondary endpoints were the proportion of patients with a partial resonse, the proportion of non-responders and efficacy on other Behçet’s disease manifestations.
The main manifestations of Behçet’s disease among the patients were genital ulcers (80%), joint involvement (73%), pseudo-folliculitis (50%), deep vein thrombosis (20%), uveitis (20%) and central nervous system involvement (13%). All of the patients had received colchicine, and 77% had been treated with steroids.
Patients experienced a median of three oral ulcers in the six months prior to the study. When the study was launched, the median oral and genital ulcer counts were two and zero, respectively, per patient. Joint manifestations were seen in 53% of patients at inclusion.
At 12 months after treatment started, 60% of patients met the complete response criteria, 33% met the partial repsonse criteria, and 10% had no response. The median number of oral ulcers decreased from two to zero between day 0 and week 12 (P<0.0001). The percentage of patients with genital ulcers compared with baseline dropped from 33% at baseline to 10% at week 12. Arthralgias were reported in 30% of patients, with a median tender joint count of four. Nineteen percent of patients were able to taper off their steroid treatments.
One patient still had a genital ulcer at the end of follow-up, and 15% of patients still reported arthraligas, with a median tender joint count of two. Of the 16 patients who used prednisone at inclusion, 37% could stop using it at the end of follow-up.
Twenty-three percent of patients reported adverse events with ustekinumab use, including headaches after treatment injection in 13% of patients, which was the most common adverse event. One patient stopped ustekinumab due to headaches; however, there were no serious adverse events in the study.
At the end of follow-up, 87% of patients were still receiving ustekinumab. In four patients, the drug was stopped at month 3 due to headaches in one patient and a Behçet’s disease flare in three patients.
The researchers concluded that ustekinumab appears to be efficient and safe for oral ulcers, but that placebo-controlled studies are needed.
Weighing In
Rheumatologists applaud research in this area because of the lack of effective treatments for oral ulcers associated with Behçet’s disease, especially treatments that don’t have major side effects.
“Refractory oral aphthous ulcerations in patients with Behçet’s disease is a clinical challenge, and the suggestion of efficacy and tolerability of an intervention with which rheumatologists are comfortable offers hope for expanding our therapeutic armamentarium in this disease,” says Robert F. Spiera, MD, Hospital for Special Surgery, New York.
“There is an unmet need not only for oral ulcer treatment, but also other manifestations of Behçet’s [disease], and hopefully, new therapies will be extended to these manifestations of Behçet’s [disease] in the future,” says Yusuf Yazici, MD, clinical associate professor of medicine, New York University Grossman School of Medicine.
In addition to the aforementioned treatments, apremilast was shown to be effective to treat Behçet’s disease-related ulcers in recent controlled studies, Dr. Saadoun says. For example, results from the phase 3 RELIEF trial with apremilast showed favorable results in Behçet’s disease patients with mouth ulcers.2 However, apremilast’s efficacy on other Behçet’s disease manifestations, including joints, remains unknown.
“There is potentially a need for other therapies for managing this less ‘organ-damaging’ manifestation of the disease, which nevertheless has an important impact on quality of life,” Dr. Spiera says.
Further research with larger studies is needed. “The study was not placebo-controlled and was small,” says Andrew Sulich, MD, Shores Rheumatology, St. Clair Shores, Mich., and assistant clinical professor, Oakland University William Beaumont School of Medicine, Rochester, Mich. “Phase 3 trials would be welcomed.”
“I think properly controlled studies are needed so we can know if ustekinumab really works for Behçet’s [disease] oral ulcers or not, before approval in the U.S. can be considered,” Dr. Yazici says.
Even with the limitations, Dr. Spiera was encouraged by the results, including how other disease manifestations showed improvement, in particular musculoskeletal symptoms and cutaneous features, as well as the overall Behçet’s disease activity score.
Of the currently used treatments in the U.S., only apremilast is approved specifically for Behçet’s disease.3 Dr. Yazici says, “Most of the data we have on these drugs are either not from randomized controlled trials or [come] from a few randomized controlled trials that, for the most part, have not shown real benefit for oral ulcers.”
Vanessa Caceres is a medical writer in Bradenton, Florida.
References
- Mirouse A, Barete S, Desbois A-C, et al. Long-term outcome of ustekinumab therapy for Behçet’s disease. Arthritis Rheumatol. 2019 Oct;71(10):1727–1732.
- Hatemi G, Mahr A, Takeno M, et al. OP0082 Apremilast for Behçet’s syndrome: A phase III randomised, placebo-controlled, double blind study (RELIEF). Ann Rheum Dis. 2018;77:91–92.
- Otezla prescribing information.