 Although scientists characterize giant cell arteritis (GCA) as an immune-mediated disease, its cause is unknown. A new study by Don Gilden, MD, and Maria Nagel, MD, of the University of Colorado School of Medicine in Aurora, Colo., suggests that an infection with the varicella zoster virus (VZV) may trigger GCA. The neurologists published their analysis of temporal arteries (TAs) in a supplement of the Journal of Infectious Diseases.1
Although scientists characterize giant cell arteritis (GCA) as an immune-mediated disease, its cause is unknown. A new study by Don Gilden, MD, and Maria Nagel, MD, of the University of Colorado School of Medicine in Aurora, Colo., suggests that an infection with the varicella zoster virus (VZV) may trigger GCA. The neurologists published their analysis of temporal arteries (TAs) in a supplement of the Journal of Infectious Diseases.1
VZV is a neurotropic virus found exclusively in humans. After causing chicken pox, the virus becomes latent in cranial nerve ganglia, dorsal root ganglia and autonomic ganglia along the entire neuroaxis. In elderly and immunocompromised individuals, VZV-specific, cell-mediated immunity declines and VZV reactivates from one or more ganglia. The reactivation results in a productive viral infection that can cause shingles. Shingles may also be complicated by VZV vasculopathy when the viral infection includes the cerebral arteries.
Originally, VZV vasculopathy was described as a large vessel stroke that resulted in hemiplegia after chicken pox or shingles. It can cause ischemic infarction of the brain and spinal cord, as well as subarachnoid and cerebral hemorrhage, aneurysm and carotid dissection. VZV vasculopathy can be unifocal or multifocal, with deep-seated and superficial infarctions. A diagnosis can be made by imaging lesions at the gray-white matter junction of the brain. Generally, both large and small arteries are involved, and most patients have mononuclear cerebrospinal fluid pleocytosis, often with red blood cells. In approximately one-third of the cases, however, cerebrospinal fluid pleocytosis and rash are absent. IgG antibody can be frequently detected in the cerebrospinal fluid, but VZV DNA is found less often.
Recently, the number of recognized vasculopathies has grown, making it somewhat difficult to diagnose and, therefore, treat these disorders effectively. Dr. Gilden and Dr. Nagel have recently expanded to the understanding that VZV vasculopathy includes transient ischemic attacks, ischemic and hemorrhagic stroke, and multifocal VZV vasculopathy. The VZV vasculopathy occurs in TAs and mimics GCA, extracranial vasculopathy, aneurysm with and without subarachnoid hemorrhage, and other disorders. All known cases of VZV vasculopathy have occurred in intracerebral arteries.2
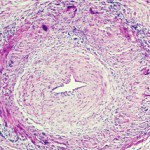
In the current study, the investigators performed immunohistochemical analyses on formalin-fixed, paraffin-embedded sections from four GCA-positive TAs and 13 normal TAs. They employed antibodies from two different species that were directed against VZV. They found VZV antigen in all four GCA-positive TAs, but no antigen in normal TAs. The VZV was primarily located in the adventitia and media. There was less VZV in the intima.
The investigators then took every section of each VZV antigen-positive TA and extracted the DNA. Despite the fact that the TA samples were formalin fixed, the researchers found VZV DNA in two of four GCA-positive, VZV antigen-positive TAs. They also found skeletal muscle attached to three of four TAs. When they analyzed the skeletal muscle, they found that two stained positive for VZV antigen and one was positive for VZV DNA.
The preliminary results suggest that antiviral agents could be combined with corticosteroids to treat GCA as a VZV-induced immunopathological disorder.
Lara C. Pullen, PhD, is a medical writer based in the Chicago area.
References
- Gilden D, Nagel M. Varicella zoster virus in temporal arteries of patients with giant cell arteritis. J Infect Dis. 2015 Jul 15;212 Suppl 1:S37–39. doi: 10.1093/infdis/jiu542.
- 2. Nagel M, Gilden D. Update on varicella zoster virus vasculopathy. Curr Infect Dis Rep. 2014 June;16(6):407. doi:10.1007/s11908-014-0407-z