 In 2021, the ACR—in concert with the Vasculitis Foundation (VF)—released four new vasculitis guidelines, one each on: 1) anti-neutrophil cytoplasmic antibody (ANCA) associated vasculitis, 2) giant cell arteritis (GCA) and Takayasu arteritis, 3) polyarteritis nodosa and 4) Kawasaki disease.1-3,13 The guideline development process is complex. For the vasculitis guidelines, this process kicked off in June 2017, when the core leadership team formed by the ACR first met in person. The ACR also convened expert and voting panels. Together, the core team and the two panels determined the project’s scope. Members of the literature review team assembled evidence using the most recent nomenclature system for vasculitis, the 2012 Chapel Hill Consensus Conference nomenclature.4 A panel of patients contributed as well. In this series, we discuss the updated recommendations with authors who contributed to each guideline. Read other installments in this series.
In 2021, the ACR—in concert with the Vasculitis Foundation (VF)—released four new vasculitis guidelines, one each on: 1) anti-neutrophil cytoplasmic antibody (ANCA) associated vasculitis, 2) giant cell arteritis (GCA) and Takayasu arteritis, 3) polyarteritis nodosa and 4) Kawasaki disease.1-3,13 The guideline development process is complex. For the vasculitis guidelines, this process kicked off in June 2017, when the core leadership team formed by the ACR first met in person. The ACR also convened expert and voting panels. Together, the core team and the two panels determined the project’s scope. Members of the literature review team assembled evidence using the most recent nomenclature system for vasculitis, the 2012 Chapel Hill Consensus Conference nomenclature.4 A panel of patients contributed as well. In this series, we discuss the updated recommendations with authors who contributed to each guideline. Read other installments in this series.
In part 2 of this series, we talk again with Sharon Chung, MD, MAS, this time about the ANCA-associated vasculitis guideline. Dr. Chung is director of the Vasculitis Clinic at the University of California, San Francisco, and served as the principal investigator of the overall vasculitis guideline effort. She also helped formulate the guidelines for ANCA-associated vasculitis.
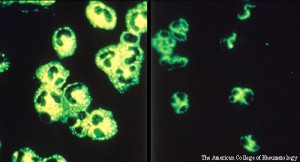
The ANCA-associated vasculitides comprise granulomatosis with polyangiitis (GPA), microscopic polyangiitis (MPA) and eosinophilic granulomatosis with polyangiitis (EGPA). These diseases affect small- and medium-sized vessels and are characterized by multisystem organ involvement. They’re often associated with an ANCA profile—typically PR3-ANCA positivity for GPA and MPO-ANCA positivity for MPA. Classically, they present with constitutional symptoms (e.g., rash, arthralgias) and some of the things I call the “scary vasculitic manifestations.” These include, but are certainly not limited to, diffuse alveolar hemorrhage (DAH), pauci-immune glomerulonephritis and mononeuritis multiplex. Patients who present with granulomatosis with polyangiitis can develop aggressive, destructive upper airway disease.
A few recommendations in the guideline will likely come as no surprise to people who have treated ANCA-associated vasculitis, such as a conditional recommendation for methotrexate in non-severe disease. The guidelines also conditionally recommend Bactrim (sulfamethoxazole and trimethoprim) for Pneumocystis pneumonia prophylaxis, but not as an explicit treatment for disease; immunosuppressive therapies are favored instead. There are also several otolaryngology recommendations.
From the guideline—Recommendations: For patients with active, severe GPA/MPA, we conditionally recommend treatment with rituximab over cyclophosphamide for remission induction. For patients with GPA/MPA who have experienced relapse with severe disease manifestations and are not receiving rituximab for remission maintenance, we conditionally recommend treatment with rituximab over cyclophosphamide for remission re-induction.
Q: What led the committee to recommend rituximab over cyclophosphamide for initial disease and for relapse? That’s my preference, but I know some people still prefer cyclophosphamide, especially with severe DAH, neurologic involvement and acute renal failure. Are there any cases where there was some disagreement about it or where you personally would still favor cyclophosphamide?
Dr. Chung: I’ll start off by saying that all of these recommendations are conditional. That means while the majority would prefer one intervention, the alternate intervention is still a reasonable consideration. A number of factors led to a conditional recommendation for rituximab over cyclophosphamide for remission induction in severe GPA or MPA.
First, I think we all recognize the toxicities of cyclophosphamide. Although we use a lot less cyclophosphamide now than we did in the past, there is still the potential for toxicity, which can have a significant impact on patients’ future fertility and malignancy risks.
Second, we had a panel of patients as part of our guideline development process, and they also expressed a preference for rituximab. I have a preference for rituximab in my clinical practice, too, because it’s a better tolerated medication when it comes to side effects, such as gastrointestinal upset and bone marrow toxicity.
We did discuss using cyclophosphamide for specific indications. As you said, some individuals are strong believers in cyclophosphamide for rapidly progressive glomerulonephritis or alveolar hemorrhage. Unfortunately, we just don’t have strong data from the clinical trials, at least, to say one intervention is better than another in those particular situations. I think decisions to use cyclophosphamide for alveolar hemorrhage and other conditions are more driven by clinical experience than by clinical trial data.
Are there certain situations where I would use cyclophosphamide over rituximab? Certainly. For example, if someone hasn’t responded to rituximab in the past, you should use cyclophosphamide first. And if I have a patient with vasculitis who has unusual manifestations—pachymeningitis, for example—I tend to reach for cyclophosphamide first because we have more experience with cyclophosphamide than we do with rituximab.
Q: What about the idea that cyclophosphamide works more quickly?
Dr. Chung: That’s an idea that’s been tossed around quite a bit. I don’t think there are good data showing rituximab has a far more delayed onset of action. As you probably know, two randomized trials have looked at rituximab vs. cyclophosphamide for severe GPA and MPA. RAVE is the one that gets talked about most because it was the larger study.5 But the second study, RITUXVAS, actually included two doses of intravenous cyclophosphamide in the rituximab group because there was concern about a delay in onset of action with rituximab.6 It was thought that including a small amount of cyclophosphamide in the beginning would prevent or ameliorate the effects of this delayed onset of action.
When I talk to nephrologists about rituximab use, they say, ‘It’s scary because you give rituximab and high-dose prednisone, hoping the high-dose prednisone will cover patients before the full effect of rituximab kicks in.’ With rituximab, I keep a close eye on our patients to make sure their disease is going in the direction we would expect with therapy.
One more note on this topic: We received complaints that we didn’t look at rituximab and cyclophosphamide together. We had a lot of comments—both when we presented this at the 2019 ACR/ARP Annual Meeting and during journal review—saying this was a limitation. At least in the U.S., using rituximab and cyclophosphamide together isn’t widely done, and that’s one of the reasons why we haven’t commented upon it. However, a clinical trial underway in Europe is looking at the efficacy of this combination therapy.
From the guideline—Recommendation: For patients with GPA/MPA who are receiving rituximab for remission maintenance, we conditionally recommend scheduled re-dosing over using ANCA titers or CD19+ B cell counts to guide re-dosing.
Q: B cell monitoring was the focus of MAINRITSAN2.7 People received less rituximab with no significant difference in flares, but the study was underpowered, in my opinion, to detect a meaningful difference, and there may have been a trend toward harm. The guideline panel recommended against B cell monitoring. Can you talk about that decision?
Dr. Chung: There was a philosophical background to that discussion. Each of the studies that have looked at rituximab for ANCA-associated vasculitis—RAVE, the original MAINRITSAN and others—have all seen flares in patients who were B cell depleted.8 Just because someone is B cell depleted does not mean they can’t relapse.
There are also philosophical thoughts about following ANCA titers, which was the other aspect of the MAINRITSAN2 trial. Most of us feel that ANCA titers are not great indicators of disease activity, and I don’t think many of us would recommend treating patients based on ANCA titers alone.
It was a potentially underpowered clinical trial with outcomes that can be hard to interpret. We must also be concerned about using these biomarkers to indicate disease activity or need for treatment. Those factors taken together led us to recommend against routinely using B cell counts or ANCA titers to dose rituximab for remission maintenance.
I usually start off with a scheduled approach to remission maintenance, whether every six months as in MAINRITSAN, or every four months based on RITAZAREM.9 But the thought of keeping patients on scheduled dosing for the rest of their lives makes me uncomfortable. At some point, I do try to figure out a way I can limit the amount of medication I’m giving to patients. When I reach that point, monitoring B cell counts or ANCA titers is a possible strategy for limiting medication exposure.
Q: Was there any controversy about the recommendation against the routine use of plasma exchange?
Dr. Chung: Plasma exchange has been looked at in two randomized trials: MEPEX and PEXIVAS; the MEPEX study pushed the PEXIVAS study to be developed.10,11 The MEPEX study showed a benefit for plasma exchange, but enrolled a very sick population—patients with a serum creatinine greater than 5.7 or 5.8 mg/dL and new-onset disease. PEXIVAS enrolled a population that wasn’t nearly as sick and didn’t have the same entry criteria. Because of that, questions have been raised about whether plasma exchange may benefit patients who have worse renal involvement.
When we first considered this recommendation, we had limited data from the PEXIVAS trial. Once that trial was published, we considered this recommendation again. When the data were reevaluated, there was a suggestion the benefit was different depending on the patient’s risk of end-stage renal disease (ESRD). If someone was at high risk of ESRD, the data suggested the benefit was much stronger than for those who were at low risk. A group of nephrologists conducted a more detailed analysis and came up with similar conclusions.
Plasma exchange does have risks. One that was hinted at in the PEXIVAS study and came out in our meta-analysis was a potential increased risk of infection. You have to weigh the potential increased risks against the potential benefit.
Q: What about people with severe DAH? The PEXIVAS trial included very few patients with DAH, but they are the patients who become very ill and wind up in the intensive care unit. We give them pulse steroids, we give them rituximab or cyclophosphamide, and then we start to get nervous because they’re not getting better. I think a lot of people reach for a plasma exchange when that happens, including myself.
Dr. Chung: When we look at the evidence, there doesn’t seem to be a decrease in mortality with plasma exchange or a decrease in relapse rates using plasma exchange for DAH, so we didn’t recommend the routine use of plasma exchange for those patients. But I do think it’s reasonable to use plasma exchange when things are not going in the right direction. And if you’ve administered high-dose glucocorticoids and induction therapy, and you’re pretty sure the patient’s not infected, it’s reasonable to start thinking about things like plasma exchange.
From the guideline—Recommendation: For patients with GPA/MPA that is refractory to remission induction therapy, we conditionally recommend adding IV immunoglobulin (IVIG) to current therapy.
Q: Can you also talk about how intravenous immunoglobulin (IVIG) was mentioned in the guidelines?
Dr. Chung: One of the reasons IVIG got incorporated is because it’s one of the few treatments that actually has a randomized controlled trial behind it. It wasn’t large, but there was a trial of IVIG for refractory disease.
I’ll be the first to say we shouldn’t be thinking about IVIG as a treatment for ANCA-associated vasculitis for the vast majority of patients, because the vast majority will have reasonable outcomes with rituximab, cyclophosphamide, methotrexate and azathioprine. But IVIG is unique in that it’s not immunosuppressive.
So, for example, if you have a pregnant patient who can’t risk exposure to cyclophosphamide and you’re nervous about giving rituximab, then IVIG is something you can use as a bridge, before using other therapies. Or you can consider IVIG in a patient who is septic from the other therapies you’ve given them, and yet still seems to have active vasculitis. A number of my patients do get IVIG, but it’s because of hypogammaglobulinemia from rituximab; it’s not for ANCA-associated vasculitis directly.
Q: What about the use of avacopan for ANCA-associated vasculitis? The phase 3 ADVOCATE trial has now been published. How will it change things?12
Dr. Chung: I can punt and say that we only considered therapies that are FDA [U.S. Food & Drug Administration] approved and that patients have access to. We could spend an entire episode talking about the ADVOCATE trial.
I will say overall though, one of the messages we received from the patient panel was that anything we can do to minimize glucocorticoid exposure and glucocorticoid toxicity is a good thing. This led to the recommendation for the lower dose glucocorticoid regimen being recommended from PEXIVAS.
I suspect if avacopan is approved, future guidelines will take a look and may come out with a recommendation supporting its use. It is premature for me to say that, but there is an overall sense that we should limit glucocorticoids for our patients, and if this allows us to do so in a safe fashion, I think many of us will be excited to do so.
 Michael Putman, MD (@EBRheum), is an assistant professor at the Medical College of Wisconsin, Wauwatosa, where he is the associate fellowship program director and the medical director of the vasculitis program.
Michael Putman, MD (@EBRheum), is an assistant professor at the Medical College of Wisconsin, Wauwatosa, where he is the associate fellowship program director and the medical director of the vasculitis program.
References
- Chung SA, Langford CA, Maz M, et al. 2021 American College of Rheumatology/Vasculitis Foundation Guideline for the Management of Antineutrophil Cytoplasmic Antibody–Associated Vasculitis. Arthritis Rheumatol and Arthritis Care Res (Hoboken). 2021 Jul 8. Online ahead of print.
- Maz M, Chung SA, Abril A, et al. 2021 American College of Rheumatology/Vasculitis Foundation Guideline for the Management of Giant Cell Arteritis and Takayasu Arteritis. Arthritis Rheumatol and Arthritis Care Res (Hoboken). 2021 Jul 8. Online ahead of print.
- Chung SA, Gorelik M, Langford CA, et al. 2021 American College of Rheumatology/Vasculitis Foundation Guideline for the Management of Polyarteritis Nodosa. Arthritis Rheumatol and Arthritis Care Res (Hoboken). 2021 Jul 8. Online ahead of print.
- Jennette JC. Overview of the 2012 revised International Chapel Hill Consensus Conference nomenclature of vasculitides. Clin Exp Nephrol. 2013 Oct;17(5):603–606.
- Stone JH, Merkel PA, Spiera R, et al. Rituximab versus cyclophosphamide for ANCA-associated vasculitis (RAVE). N Engl J Med. 2010 Jul 15;363(3):221–232.
- Jones RB, Furuta S, Tervaert JWC, et al. Rituximab versus cyclophosphamide in ANCA-associated renal vasculitis: 2-year results of a randomised trial. Ann Rheum Dis. 2015 Jun;74(6):1178–1182.
- Charles P, Terrier B, Perrodeau É, et al. Comparison of individually tailored versus fixed-schedule rituximab regimen to maintain ANCA-associated vasculitis remission: Results of a multicentre, randomised controlled, phase III trial (MAINRITSAN2). Ann Rheum Dis. 2018 Aug;77(8):1143–1149.
- Guillevin L, Pagnoux C, Karras A, et al. Rituximab versus azathioprine for maintenance in ANCA-associated vasculitis. N Engl J Med. 2014 Nov 6;371(19):1771–1780.
- Gopaluni S, Smith RM, Lewin M, et al. Rituximab versus azathioprine as therapy for maintenance of remission for anti-neutrophil cytoplasm antibody-associated vasculitis (RITAZAREM): Study protocol for a randomized controlled trial. Trials. 2017 Mar 7;18(1):112.
- Jayne DRW, Gaskin G, Rasmussen N, et al. Randomized trial of plasma exchange or high-dosage methylprednisolone as adjunctive therapy for severe renal vasculitis (MEPEX). J Am Soc Nephrol. 2007 Jul;18(7):2180–2188.
- Walsh M, Merkel PA, Peh CA, et al. Plasma exchange and glucocorticoids in severe ANCA-associated vasculitis. N Engl J Med. 2020 Feb 13;382(7):622–631.
- Jayne DRW, Merkel PA, Schall TJ, Bekker P. Avacopan for the treatment of ANCA-associated vasculitis. N Engl J Med. 2021 Feb 18;384(7):599–609.
- Gorelik M, Chung SA, Ardalan K, et al. 2021 American College of Rheumatology/Vasculitis Foundation Guideline for the Management of Kawasaki Disease. Arthritis Rheumatol. 2022 Apr; 74(4):586–596; and Arthritis Care Res (Hoboken). 2022 Apr;74(4):538–548.


